Ghrelin
Ghrelin (/ˈɡrɛlɪn/; or lenomorelin, INN) is a hormone primarily produced by enteroendocrine cells of the gastrointestinal tract, especially the stomach,[5][6] and is often called a "hunger hormone" because it increases the drive to eat.[6] Blood levels of ghrelin are highest before meals when hungry, returning to lower levels after mealtimes.[6][7] Ghrelin may help prepare for food intake[6][8] by increasing gastric motility and stimulating the secretion of gastric acid.[6]
Ghrelin activates cells in the anterior pituitary gland and hypothalamic arcuate nucleus,[6][9] including neuropeptide Y neurons that initiate appetite.[6][10] Ghrelin stimulates brain structures having a specific receptor – the growth hormone secretagogue receptor 1A (GHSR-1A).[6][11] Ghrelin also participates in regulation of reward cognition,[12] learning and memory, the sleep-wake cycle, taste sensation, reward behavior, and glucose metabolism.[6][13][14]
History and name
[edit]Ghrelin was discovered after the ghrelin receptor (called growth hormone secretagogue type 1A receptor or GHS-R) was determined in 1999.[6] The hormone name is based on its role as a growth hormone-releasing peptide, with reference to the Proto-Indo-European root gʰre-, meaning "to grow".[6]
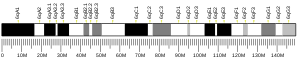
Gene, transcription products, and structure
[edit]
The GHRL gene produces mRNA which has four exons. Five products arise: the first is the 117-amino acid preproghrelin. It is homologous to promotilin; both are members of the motilin family. It is cleaved to produce proghrelin which is cleaved to produce an unacylated 28-amino acid ghrelin and an acylated C-ghrelin. Obestatin is presumed to be cleaved from C-ghrelin.[15]
Ghrelin only becomes active when caprylic (octanoic) acid is linked posttranslationally to serine at the 3-position by the enzyme ghrelin O-acyltransferase (GOAT) to form a proteolipid. It is located on the cell membrane of ghrelin cells in the stomach and pancreas.[16] The non-octanoylated form is desacyl ghrelin. It does not activate the GHS-R receptor but does have other effects: cardiac,[17] anti-ghrelin,[18] appetite stimulation,[19] and inhibition of hepatic glucose output.[20] Side-chains other than octanoyl have also been observed: these can also trigger the ghrelin receptor.[21] In particular, decanoyl ghrelin has been found to constitute a significant portion of circulating ghrelin in mice, but as of 2011 its presence in humans has not been established.[22]
Ghrelin cells
[edit]Alternative names
[edit]The ghrelin cell is also known as an A-like cell (pancreas), X-cell (for unknown function), X/A-like cell (rats), Epsilon cell (pancreas), P/D sub 1 cell (humans) and Gr cell (abbreviation for ghrelin cell).[23]
Location
[edit]Ghrelin cells are found mainly in the stomach[24] and duodenum, but also in the jejunum, lungs, pancreatic islets,[25] gonads, adrenal cortex, placenta, and kidney. It has also been shown that ghrelin is produced locally in the brain.[26] Additionally, research suggests that ghrelin may be produced in the myocardium and have an 'autocrine/ paracrine' like effect within the heart.[27]
Ghrelin cells are also found in oxyntic glands (20% of cells),[28] pyloric glands, and small intestine.
Features
[edit]They are ovoid cells with granules.[29] They have gastrin receptors.[30] Some produce nesfatin-1.[31] Ghrelin cells are not terminally differentiated in the pancreas: they are progenitor cells that can give rise to A-cells, PP cells and Beta-cells there.[32]
Function and mechanism of action
[edit]Ghrelin is a participant in regulating the complex process of energy homeostasis which adjusts both energy input – by adjusting hunger signals – and energy output – by adjusting the proportion of energy going to ATP production, fat storage, glycogen storage, and short-term heat loss. The net result of these processes is reflected in body weight, and is under continuous monitoring and adjustment based on metabolic signals and needs. At any given moment in time, it may be in equilibrium or disequilibrium. Gastric-brain communication is an essential part of energy homeostasis, and several communication pathways are probable, including the gastric intracellular mTOR/S6K1 pathway mediating the interaction among ghrelin, nesfatin and endocannabinoid gastric systems,[33] and both afferent and efferent vagal signals.
Ghrelin and synthetic ghrelin mimetics (growth hormone secretagogues) increase body weight and fat mass[34][35][36] by triggering receptors in the arcuate nucleus[9] that include neuropeptide Y (NPY) and agouti-related protein (AgRP) neurons.[37][10] Ghrelin-responsiveness of these neurons is both leptin- and insulin-sensitive.[38] Ghrelin reduces the sensitivity of gastric vagal afferents, so they are less sensitive to gastric distension.[39]
In addition to its function in energy homeostasis, ghrelin also activates the cholinergic–dopaminergic reward link in inputs to the ventral tegmental area and in the mesolimbic pathway,[40] a circuit that communicates the hedonic and reinforcing aspects of natural rewards,[13] such as food and addictive drugs such as ethanol.[38][41][42] Ghrelin receptors are located on neurons in this circuit.[13][12] Hypothalamic ghrelin signalling is required for reward from alcohol[43] and palatable/rewarding foods.[44][45]
Ghrelin has been linked to inducing appetite and feeding behaviors. Circulating ghrelin levels are the highest right before a meal and the lowest right after.[46][47] Injections of ghrelin in both humans and rats have been shown to increase food intake in a dose-dependent manner.[48] So the more ghrelin that is injected the more food that is consumed. However, ghrelin does not increase meal size, only meal number.[49] Ghrelin injections also increase an animal's motivation to seek out food, behaviors including increased sniffing, foraging for food, and hoarding food. Body weight is regulated through energy balance, the amount of energy taken in versus the amount of energy expended over an extended period of time. Studies have shown that ghrelin levels are positively correlated with weight. This data suggests that ghrelin functions as an adiposity signal, a messenger between the body's energy stores and the brain.[8]
Blood levels
[edit]Blood levels are in the pmol/L or fmol/mL range. Both active and total ghrelin can be measured.[50] Circulating ghrelin concentrations rise before eating and fall afterward,[46] more strongly in response to protein and carbohydrate than to lipids.[22] The plasma ghrelin-like immunoreactivity concentration measured with a particular radioimmunoassay in a typical human is 166.0 + 10.1 fmol/mL. Serum ghrelin concentrations tend to increase in age and vary throughout the day, with values peaking while one is asleep.[51]
Ghrelin receptor
[edit]The ghrelin receptor GHS-R1a (a splice-variant of the growth hormone secretagogue receptor, with the GHS-R1b splice being inactive) is involved in mediating a wide variety of biological effects of ghrelin, including: stimulation of growth hormone release, increase in hunger, modulation of glucose and lipid metabolism, regulation of gastrointestinal motility and secretion, protection of neuronal and cardiovascular cells, and regulation of immune function.[52] They are present in high density in the hypothalamus and pituitary, on the vagus nerve (on both afferent cell bodies and efferent nerve endings) and throughout the gastrointestinal tract.[16][39]
Locations of action
[edit]Glucose metabolism
[edit]The entire ghrelin system (dAG, AG, GHS-R and GOAT) has a gluco-regulatory action.[53]
Sleep
[edit]Preliminary research indicates that ghrelin participates in the regulation of circadian rhythms.[6] A review reported finding strong evidence that sleep restriction affected ghrelin or leptin levels, or energy expenditure.[54]
Reproductive system
[edit]Ghrelin has inhibitory effects on gonadotropin-releasing hormone (GnRH) secretion. It may cause decreased fertility.[55]
Fetus and neonate
[edit]Ghrelin is produced early by the fetal lung and promotes lung growth.[56] Umbilical cord blood levels of ghrelin show a correlation between ghrelin levels and birth weight.[50]
Cardiovascular system
[edit]Ghrelin functions as a cardio-protective peptide by being an anti-inflammatory agent, promoting angiogenesis, inhibiting arrhythmia, and improving heart failure.[57]
Immune system
[edit]Ghrelin has a diverse immunoregulatory role mediating the release of anti-inflammatory cytokines such as IL-4 and 10 along with TGF-β while reducing pro-inflammatory cytokines such as TNF-α, INF-γ, and IL-1β from various immunologically competent cells in vitro and in vivo. [58] Additionally, Ghrelin and its endogenous receptor, GHSR1a, along with GOAT are expressed in primary immune tissues such as the spleen and thymus where it has a role in modulating interactions between metabolic state and inflammation, mediating energy balance homeostasis.[59]
Stress/ Hypothalamic-pituitary-adrenal (HPA) axis
[edit]GHSR1A, Ghrelin's endogenous receptor, is expressed within the hypothalamus including the arcuate nucleus, but not in the paraventricular nucleus (PVN) where ghrelin has been found to indirectly affect HPA axis function via neighboring corticotropin releasing hormone (CRH) neurons.[60] Studies regarding how ghrelin affects cortisol and adrenocorticotropic hormone (ACTH) secretion along with how cortisol and ACTH levels affect ghrelin are inconsistent as different psychological and physical stressors within in vivo studies have produced a myriad of results as the underlying mechanisms are still not understood well.[61]
Role(s) in disease
[edit]Gastric bypass surgery
[edit]Gastric bypass surgery not only reduces gut capacity for food, but also lowers ghrelin levels compared to both lean people and those who lost weight through dieting.[62][63] Studies have not clarified whether ghrelin levels return to normal in people who had gastric bypass surgery after weight loss has stabilized.[64] Gastric bypass surgery involving vertical-sleeve gastrectomy reduces plasma ghrelin levels by about 60% in the long term.[65]
Anorexia and obesity
[edit]Ghrelin levels in the plasma of obese individuals are lower than those in leaner individuals,[62][66] suggesting that ghrelin does not contribute to obesity, except in the cases of Prader–Willi syndrome-induced obesity, where high ghrelin levels are correlated with increased food intake.[67][68] Those with anorexia nervosa have high plasma levels of ghrelin[69] compared to both the constitutionally thin and normal-weight controls.[70][71] The level of ghrelin increases during the time of day from midnight to dawn in thinner people, which suggests there is a flaw in the circadian rhythm of obese individuals.[72] Ghrelin levels are high in people with cancer-induced cachexia.[73] There is insufficient evidence to conclude either for or against use of ghrelin in managing cachexia associated with cancer.[74]
Effects on cardiovascular system
[edit]Ghrelin has been theorized to have protective effects on the cardiovascular system. Studies have shown that in mice models of myocardial infarction (MI) with knock-outs of ghrelin, subjects with no endogenous ghrelin production had a significantly increased mortality rate along with worse metrics in terms of cardiac sympathetic activity and systolic function when compared to wild-type subjects.[57] with exogenous ghrelin being shown to improve heart function in rodent models of chronic heart failure [57] and improved ventricular remodeling in post-MI rats.[27]
See also
[edit]References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000157017 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000064177 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Kojima M, Hosoda H, Date Y, Nakazato M, Matsuo H, Kangawa K (December 1999). "Ghrelin is a growth-hormone-releasing acylated peptide from stomach". Nature. 402 (6762): 656–660. Bibcode:1999Natur.402..656K. doi:10.1038/45230. PMID 10604470. S2CID 753383.
- ^ a b c d e f g h i j k l Müller TD, Nogueiras R, Andermann ML, Andrews ZB, Anker SD, Argente J, et al. (June 2015). "Ghrelin". Molecular Metabolism. 4 (6): 437–460. doi:10.1016/j.molmet.2015.03.005. PMC 4443295. PMID 26042199.
- ^ Cummings DE, Purnell JQ, Frayo RS, Schmidova K, Wisse BE, Weigle DS (August 2001). "A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans". Diabetes. 50 (8): 1714–1719. doi:10.2337/diabetes.50.8.1714. PMID 11473029.
- ^ a b Schwartz MW, Woods SC, Porte D, Seeley RJ, Baskin DG (April 2000). "Central nervous system control of food intake". Nature. 404 (6778): 661–671. doi:10.1038/35007534. PMID 10766253. S2CID 205005718.
- ^ a b Dickson SL, Leng G, Robinson IC (March 1993). "Systemic administration of growth hormone-releasing peptide activates hypothalamic arcuate neurons". Neuroscience. 53 (2): 303–306. doi:10.1016/0306-4522(93)90197-n. PMID 8492908. S2CID 9757253.
- ^ a b Dickson SL, Luckman SM (February 1997). "Induction of c-fos messenger ribonucleic acid in neuropeptide Y and growth hormone (GH)-releasing factor neurons in the rat arcuate nucleus following systemic injection of the GH secretagogue, GH-releasing peptide-6". Endocrinology. 138 (2): 771–777. doi:10.1210/endo.138.2.4907. PMID 9003014.
- ^ Howard AD, Feighner SD, Cully DF, Arena JP, Liberator PA, Rosenblum CI, et al. (August 1996). "A receptor in pituitary and hypothalamus that functions in growth hormone release". Science. 273 (5277): 974–977. Bibcode:1996Sci...273..974H. doi:10.1126/science.273.5277.974. PMID 8688086. S2CID 32192383.
- ^ a b Nestler EJ, Hyman SE, Holtzman DM, Malenka RC (2015). "Neural and Neuroendocrine Control of the Internal Milieu". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (3rd ed.). New York: McGraw-Hill Medical. pp. 245–267. ISBN 9780071827690.
- ^ a b c Dickson SL, Egecioglu E, Landgren S, Skibicka KP, Engel JA, Jerlhag E (June 2011). "The role of the central ghrelin system in reward from food and chemical drugs" (PDF). Molecular and Cellular Endocrinology. 340 (1): 80–87. doi:10.1016/j.mce.2011.02.017. hdl:2077/26318. PMID 21354264. S2CID 206815322.
Whereas ghrelin emerged as a stomach-derived hormone involved in energy balance, hunger and meal initiation via hypothalamic circuits, it now seems clear that it also has a role in motivated reward-driven behaviours via activation of the so-called "cholinergic-dopaminergic reward link".
- ^ Le Moal M (2002). "Mesocorticolimbic Dopaminergic Neurons". In Davis KL, Charney D, Coyle JT, Nemeroff C (eds.). Neuropsychopharmacology : the fifth generation of progress : an official publication of the American College of Neuropsychopharmacology (5th ed.). Philadelphia, Pa.: Lippincott Williams & Wilkins. ISBN 978-0781728379. Archived from the original on 5 February 2018. Retrieved 21 May 2014.
- ^ Seim I, Amorim L, Walpole C, Carter S, Chopin LK, Herington AC (January 2010). "Ghrelin gene-related peptides: multifunctional endocrine / autocrine modulators in health and disease". Clinical and Experimental Pharmacology & Physiology. 37 (1): 125–131. doi:10.1111/j.1440-1681.2009.05241.x. PMID 19566830. S2CID 21657818.
- ^ a b Castañeda TR, Tong J, Datta R, Culler M, Tschöp MH (January 2010). "Ghrelin in the regulation of body weight and metabolism". Frontiers in Neuroendocrinology. 31 (1): 44–60. doi:10.1016/j.yfrne.2009.10.008. PMID 19896496. S2CID 23820027.
- ^ Bedendi I, Alloatti G, Marcantoni A, Malan D, Catapano F, Ghé C, et al. (August 2003). "Cardiac effects of ghrelin and its endogenous derivatives des-octanoyl ghrelin and des-Gln14-ghrelin". European Journal of Pharmacology. 476 (1–2): 87–95. doi:10.1016/S0014-2999(03)02083-1. hdl:2318/125949. PMID 12969753. S2CID 20542064.
- ^ Broglio F, Gottero C, Prodam F, Gauna C, Muccioli G, Papotti M, et al. (June 2004). "Non-acylated ghrelin counteracts the metabolic but not the neuroendocrine response to acylated ghrelin in humans". The Journal of Clinical Endocrinology and Metabolism. 89 (6): 3062–3065. doi:10.1210/jc.2003-031964. PMID 15181099.
- ^ Toshinai K, Yamaguchi H, Sun Y, Smith RG, Yamanaka A, Sakurai T, et al. (May 2006). "Des-acyl ghrelin induces food intake by a mechanism independent of the growth hormone secretagogue receptor". Endocrinology. 147 (5): 2306–2314. doi:10.1210/en.2005-1357. PMID 16484324.
- ^ Gauna C, Delhanty PJ, Hofland LJ, Janssen JA, Broglio F, Ross RJ, et al. (February 2005). "Ghrelin stimulates, whereas des-octanoyl ghrelin inhibits, glucose output by primary hepatocytes". The Journal of Clinical Endocrinology and Metabolism. 90 (2): 1055–1060. doi:10.1210/jc.2004-1069. PMID 15536157.
- ^ Korbonits M, Goldstone AP, Gueorguiev M, Grossman AB (April 2004). "Ghrelin--a hormone with multiple functions". Frontiers in Neuroendocrinology. 25 (1): 27–68. doi:10.1016/j.yfrne.2004.03.002. PMID 15183037. S2CID 24821233.
- ^ a b Stengel A, Taché Y (June 2011). "Interaction between gastric and upper small intestinal hormones in the regulation of hunger and satiety: ghrelin and cholecystokinin take the central stage". Current Protein & Peptide Science. 12 (4): 293–304. doi:10.2174/138920311795906673. PMC 3670092. PMID 21428875.
- ^ Zigman JM, Nakano Y, Coppari R, Balthasar N, Marcus JN, Lee CE, et al. (December 2005). "Mice lacking ghrelin receptors resist the development of diet-induced obesity". The Journal of Clinical Investigation. 115 (12): 3564–3572. doi:10.1172/JCI26002. PMC 1297251. PMID 16322794.
- ^ Ariyasu H, Takaya K, Tagami T, Ogawa Y, Hosoda K, Akamizu T, et al. (October 2001). "Stomach is a major source of circulating ghrelin, and feeding state determines plasma ghrelin-like immunoreactivity levels in humans". The Journal of Clinical Endocrinology and Metabolism. 86 (10): 4753–4758. doi:10.1210/jcem.86.10.7885. PMID 11600536.
- ^ Suckale J, Solimena M (May 2008). "Pancreas islets in metabolic signaling--focus on the beta-cell". Frontiers in Bioscience. 13 (13): 7156–7171. doi:10.2741/3218. PMID 18508724. S2CID 646106.
- ^ Ferrini F, Salio C, Lossi L, Merighi A (March 2009). "Ghrelin in central neurons". Current Neuropharmacology. 7 (1): 37–49. doi:10.2174/157015909787602779. PMC 2724662. PMID 19721816.
- ^ a b Zhang G, Yin X, Qi Y, Pendyala L, Chen J, Hou D, Tang C (February 2010). "Ghrelin and cardiovascular diseases". Current Cardiology Reviews. 6 (1): 62–70. doi:10.2174/157340310790231662. PMC 2845796. PMID 21286280.
- ^ Simonsson M, Eriksson S, Håkanson R, Lind T, Lönroth H, Lundell L, et al. (November 1988). "Endocrine cells in the human oxyntic mucosa. A histochemical study". Scandinavian Journal of Gastroenterology. 23 (9): 1089–1099. doi:10.3109/00365528809090174. PMID 2470131.
- ^ Grube D, Forssmann WG (November 1979). "Morphology and function of the entero-endocrine cells". Hormone and Metabolic Research = Hormon- und Stoffwechselforschung = Hormones et Métabolisme. 11 (11): 589–606. doi:10.1055/s-0028-1092785. PMID 94030. S2CID 40287472.
- ^ Fukumoto K, Nakahara K, Katayama T, Miyazatao M, Kangawa K, Murakami N (September 2008). "Synergistic action of gastrin and ghrelin on gastric acid secretion in rats". Biochemical and Biophysical Research Communications. 374 (1): 60–63. doi:10.1016/j.bbrc.2008.06.114. PMID 18611393.
- ^ Inhoff T, Stengel A, Peter L, Goebel M, Taché Y, Bannert N, et al. (February 2010). "Novel insight in distribution of nesfatin-1 and phospho-mTOR in the arcuate nucleus of the hypothalamus of rats". Peptides. 31 (2): 257–262. doi:10.1016/j.peptides.2009.11.024. PMC 4043136. PMID 19961888.
- ^ Arnes L, Hill JT, Gross S, Magnuson MA, Sussel L (2012). "Ghrelin expression in the mouse pancreas defines a unique multipotent progenitor population". PLOS ONE. 7 (12): e52026. Bibcode:2012PLoSO...752026A. doi:10.1371/journal.pone.0052026. PMC 3520898. PMID 23251675.
- ^ Folgueira C, Seoane LM, Casanueva FF (2014). "The Brain-Stomach Connection". In Delhanty PJD, van der Lely AJ (eds.). How Gut and Brain Control Metabolism. Frontiers of Hormone Research. Vol. 42. Basel: Karger. pp. 83–92. doi:10.1159/000358316. ISBN 978-3-318-02638-2. PMID 24732927.
- ^ Lall S, Tung LY, Ohlsson C, Jansson JO, Dickson SL (January 2001). "Growth hormone (GH)-independent stimulation of adiposity by GH secretagogues". Biochemical and Biophysical Research Communications. 280 (1): 132–138. doi:10.1006/bbrc.2000.4065. PMID 11162489.
- ^ Tschöp M, Smiley DL, Heiman ML (October 2000). "Ghrelin induces adiposity in rodents". Nature. 407 (6806): 908–913. Bibcode:2000Natur.407..908T. doi:10.1038/35038090. PMID 11057670. S2CID 4564644.
- ^ Chebani Y, Marion C, Zizzari P, Chettab K, Pastor M, Korostelev M, et al. (April 2016). "Enhanced responsiveness of Ghsr Q343X rats to ghrelin results in enhanced adiposity without increased appetite" (PDF). Science Signaling. 9 (424): ra39. doi:10.1126/scisignal.aae0374. PMID 27095593. S2CID 29245906.
- ^ Chen HY, Trumbauer ME, Chen AS, Weingarth DT, Adams JR, Frazier EG, et al. (June 2004). "Orexigenic action of peripheral ghrelin is mediated by neuropeptide Y and agouti-related protein". Endocrinology. 145 (6): 2607–2612. doi:10.1210/en.2003-1596. PMID 14962995.
- ^ a b Hewson AK, Tung LY, Connell DW, Tookman L, Dickson SL (December 2002). "The rat arcuate nucleus integrates peripheral signals provided by leptin, insulin, and a ghrelin mimetic". Diabetes. 51 (12): 3412–3419. doi:10.2337/diabetes.51.12.3412. PMID 12453894.
- ^ a b Page AJ, Slattery JA, Milte C, Laker R, O'Donnell T, Dorian C, et al. (May 2007). "Ghrelin selectively reduces mechanosensitivity of upper gastrointestinal vagal afferents". American Journal of Physiology. Gastrointestinal and Liver Physiology. 292 (5): G1376–G1384. doi:10.1152/ajpgi.00536.2006. PMID 17290011. S2CID 10681559.
- ^ Naleid AM, Grace MK, Cummings DE, Levine AS (November 2005). "Ghrelin induces feeding in the mesolimbic reward pathway between the ventral tegmental area and the nucleus accumbens". Peptides. 26 (11): 2274–2279. doi:10.1016/j.peptides.2005.04.025. PMID 16137788. S2CID 25619880.
- ^ Jerlhag E, Egecioglu E, Dickson SL, Andersson M, Svensson L, Engel JA (March 2006). "Ghrelin stimulates locomotor activity and accumbal dopamine-overflow via central cholinergic systems in mice: implications for its involvement in brain reward". Addiction Biology. 11 (1): 45–54. doi:10.1111/j.1369-1600.2006.00002.x. PMID 16759336. S2CID 33650732.
- ^ Jerlhag E, Egecioglu E, Dickson SL, Douhan A, Svensson L, Engel JA (March 2007). "Ghrelin administration into tegmental areas stimulates locomotor activity and increases extracellular concentration of dopamine in the nucleus accumbens". Addiction Biology. 12 (1): 6–16. doi:10.1111/j.1369-1600.2006.00041.x. PMID 17407492. S2CID 22556527.
- ^ Jerlhag E, Egecioglu E, Landgren S, Salomé N, Heilig M, Moechars D, et al. (July 2009). "Requirement of central ghrelin signaling for alcohol reward". Proceedings of the National Academy of Sciences of the United States of America. 106 (27): 11318–11323. Bibcode:2009PNAS..10611318J. doi:10.1073/pnas.0812809106. PMC 2703665. PMID 19564604.
- ^ Egecioglu E, Jerlhag E, Salomé N, Skibicka KP, Haage D, Bohlooly-Y M, et al. (July 2010). "Ghrelin increases intake of rewarding food in rodents". Addiction Biology. 15 (3): 304–311. doi:10.1111/j.1369-1600.2010.00216.x. PMC 2901520. PMID 20477752.
- ^ Skibicka KP, Hansson C, Egecioglu E, Dickson SL (January 2012). "Role of ghrelin in food reward: impact of ghrelin on sucrose self-administration and mesolimbic dopamine and acetylcholine receptor gene expression". Addiction Biology. 17 (1): 95–107. doi:10.1111/j.1369-1600.2010.00294.x. PMC 3298643. PMID 21309956.
- ^ a b Tolle V, Bassant MH, Zizzari P, Poindessous-Jazat F, Tomasetto C, Epelbaum J, Bluet-Pajot MT (April 2002). "Ultradian rhythmicity of ghrelin secretion in relation with GH, feeding behavior, and sleep-wake patterns in rats". Endocrinology. 143 (4): 1353–1361. doi:10.1210/endo.143.4.8712. PMID 11897692.
- ^ Cummings DE, Frayo RS, Marmonier C, Aubert R, Chapelot D (August 2004). "Plasma ghrelin levels and hunger scores in humans initiating meals voluntarily without time- and food-related cues". American Journal of Physiology. Endocrinology and Metabolism. 287 (2): E297–E304. doi:10.1152/ajpendo.00582.2003. PMID 15039149. S2CID 14197143.
- ^ Wren AM, Small CJ, Ward HL, Murphy KG, Dakin CL, Taheri S, et al. (November 2000). "The novel hypothalamic peptide ghrelin stimulates food intake and growth hormone secretion". Endocrinology. 141 (11): 4325–4328. doi:10.1210/endo.141.11.7873. PMID 11089570.
- ^ Faulconbridge LF, Cummings DE, Kaplan JM, Grill HJ (September 2003). "Hyperphagic effects of brainstem ghrelin administration". Diabetes. 52 (9): 2260–2265. doi:10.2337/diabetes.52.9.2260. PMID 12941764.
- ^ a b Yokota I, Kitamura S, Hosoda H, Kotani Y, Kangawa K (April 2005). "Concentration of the n-octanoylated active form of ghrelin in fetal and neonatal circulation". Endocrine Journal. 52 (2): 271–276. doi:10.1507/endocrj.52.271. PMID 15863960.
- ^ Ibrahim Abdalla MM (August 2015). "Ghrelin - Physiological Functions and Regulation". European Endocrinology. 11 (2): 90–95. doi:10.17925/EE.2015.11.02.90. PMC 5819073. PMID 29632576.
- ^ Yin Y, Li Y, Zhang W (March 2014). "The growth hormone secretagogue receptor: its intracellular signaling and regulation". International Journal of Molecular Sciences. 15 (3): 4837–4855. doi:10.3390/ijms15034837. PMC 3975427. PMID 24651458.
- ^ Heppner KM, Tong J (July 2014). "Mechanisms in endocrinology: regulation of glucose metabolism by the ghrelin system: multiple players and multiple actions". European Journal of Endocrinology. 171 (1): R21–R32. doi:10.1530/EJE-14-0183. PMID 24714083.
- ^ Zhu B, Shi C, Park CG, Zhao X, Reutrakul S (June 2019). "Effects of sleep restriction on metabolism-related parameters in healthy adults: A comprehensive review and meta-analysis of randomized controlled trials". Sleep Medicine Reviews. 45: 18–30. doi:10.1016/j.smrv.2019.02.002. PMID 30870662. S2CID 78091930.
- ^ Comninos AN, Jayasena CN, Dhillo WS (2014). "The relationship between gut and adipose hormones, and reproduction". Human Reproduction Update. 20 (2): 153–174. doi:10.1093/humupd/dmt033. PMID 24173881.
- ^ Santos M, Bastos P, Gonzaga S, Roriz JM, Baptista MJ, Nogueira-Silva C, et al. (April 2006). "Ghrelin expression in human and rat fetal lungs and the effect of ghrelin administration in nitrofen-induced congenital diaphragmatic hernia". Pediatric Research. 59 (4 Pt 1): 531–537. doi:10.1203/01.pdr.0000202748.66359.a9. hdl:1822/67942. PMID 16549524.
- ^ a b c Hosoda H (August 2022). "Effect of Ghrelin on the Cardiovascular System". Biology. 11 (8): 1190. doi:10.3390/biology11081190. PMC 9405061. PMID 36009817.
- ^ Pereira JA, da Silva FC, de Moraes-Vieira PM (2017). "The Impact of Ghrelin in Metabolic Diseases: An Immune Perspective". Journal of Diabetes Research. 2017: 4527980. doi:10.1155/2017/4527980. PMC 5610818. PMID 29082258.
- ^ Chowen JA, Argente J (July 2017). "Ghrelin: A Link Between Energy Homeostasis and the Immune System". Endocrinology. 158 (7): 2077–2081. doi:10.1210/en.2017-00350. PMID 28881864.
- ^ Spencer SJ, Emmerzaal TL, Kozicz T, Andrews ZB (July 2015). "Ghrelin's Role in the Hypothalamic-Pituitary-Adrenal Axis Stress Response: Implications for Mood Disorders". Biological Psychiatry. 78 (1): 19–27. doi:10.1016/j.biopsych.2014.10.021. PMID 25534754. S2CID 38370890.
- ^ Fritz EM, Singewald N, De Bundel D (27 October 2020). "The Good, the Bad and the Unknown Aspects of Ghrelin in Stress Coping and Stress-Related Psychiatric Disorders". Frontiers in Synaptic Neuroscience. 12: 594484. doi:10.3389/fnsyn.2020.594484. PMC 7652849. PMID 33192444.
- ^ a b Müller TD, Nogueiras R, Andermann ML, Andrews ZB, Anker SD, Argente J, et al. (June 2015). "Ghrelin". Molecular Metabolism. 4 (6): 437–460. doi:10.1016/j.molmet.2015.03.005. PMC 4443295. PMID 26042199.
- ^ Cummings DE, Weigle DS, Frayo RS, Breen PA, Ma MK, Dellinger EP, Purnell JQ (May 2002). "Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery". The New England Journal of Medicine. 346 (21): 1623–1630. doi:10.1056/NEJMoa012908. PMID 12023994.
- ^ Cummings DE, Shannon MH (July 2003). "Ghrelin and gastric bypass: is there a hormonal contribution to surgical weight loss?". The Journal of Clinical Endocrinology and Metabolism. 88 (7): 2999–3002. doi:10.1210/jc.2003-030705. PMID 12843132.
- ^ Bohdjalian A, Langer FB, Shakeri-Leidenmühler S, Gfrerer L, Ludvik B, Zacherl J, Prager G (May 2010). "Sleeve gastrectomy as sole and definitive bariatric procedure: 5-year results for weight loss and ghrelin". Obesity Surgery. 20 (5): 535–540. doi:10.1007/s11695-009-0066-6. PMID 20094819. S2CID 207303352.
- ^ Shiiya T, Nakazato M, Mizuta M, Date Y, Mondal MS, Tanaka M, et al. (January 2002). "Plasma ghrelin levels in lean and obese humans and the effect of glucose on ghrelin secretion". The Journal of Clinical Endocrinology and Metabolism. 87 (1): 240–244. doi:10.1210/jcem.87.1.8129. PMID 11788653.
- ^ Goldstone AP, Thomas EL, Brynes AE, Castroman G, Edwards R, Ghatei MA, et al. (April 2004). "Elevated fasting plasma ghrelin in prader-willi syndrome adults is not solely explained by their reduced visceral adiposity and insulin resistance". The Journal of Clinical Endocrinology and Metabolism. 89 (4): 1718–1726. doi:10.1210/jc.2003-031118. PMID 15070936.
- ^ DelParigi A, Tschöp M, Heiman ML, Salbe AD, Vozarova B, Sell SM, et al. (December 2002). "High circulating ghrelin: a potential cause for hyperphagia and obesity in prader-willi syndrome". The Journal of Clinical Endocrinology and Metabolism. 87 (12): 5461–5464. doi:10.1210/jc.2002-020871. PMID 12466337.
- ^ Misra M, Klibanski A (July 2014). "Endocrine consequences of anorexia nervosa". The Lancet. Diabetes & Endocrinology. 2 (7): 581–592. doi:10.1016/S2213-8587(13)70180-3. PMC 4133106. PMID 24731664.
- ^ Tolle V, Kadem M, Bluet-Pajot MT, Frere D, Foulon C, Bossu C, et al. (January 2003). "Balance in ghrelin and leptin plasma levels in anorexia nervosa patients and constitutionally thin women". The Journal of Clinical Endocrinology and Metabolism. 88 (1): 109–116. doi:10.1210/jc.2002-020645. PMID 12519838.
- ^ Germain N, Galusca B, Le Roux CW, Bossu C, Ghatei MA, Lang F, et al. (April 2007). "Constitutional thinness and lean anorexia nervosa display opposite concentrations of peptide YY, glucagon-like peptide 1, ghrelin, and leptin". The American Journal of Clinical Nutrition. 85 (4): 967–971. doi:10.1093/ajcn/85.4.967. PMID 17413094.
- ^ Yildiz BO, Suchard MA, Wong ML, McCann SM, Licinio J (July 2004). "Alterations in the dynamics of circulating ghrelin, adiponectin, and leptin in human obesity". Proceedings of the National Academy of Sciences of the United States of America. 101 (28): 10434–10439. Bibcode:2004PNAS..10110434Y. doi:10.1073/pnas.0403465101. PMC 478601. PMID 15231997.
- ^ Garcia JM, Garcia-Touza M, Hijazi RA, Taffet G, Epner D, Mann D, et al. (May 2005). "Active ghrelin levels and active to total ghrelin ratio in cancer-induced cachexia". The Journal of Clinical Endocrinology and Metabolism. 90 (5): 2920–2926. doi:10.1210/jc.2004-1788. PMID 15713718.
- ^ Khatib MN, Shankar AH, Kirubakaran R, Gaidhane A, Gaidhane S, Simkhada P, Quazi Syed Z (February 2018). "Ghrelin for the management of cachexia associated with cancer". The Cochrane Database of Systematic Reviews. 2 (2): CD012229. doi:10.1002/14651858.cd012229.pub2. PMC 6491219. PMID 29489032.


 French
French Deutsch
Deutsch