Tunneling nanotube
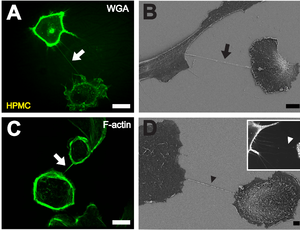
B Depiction of a TNT (black arrow) between two cells with scanning electron microscopy. Scale bar: 10 μm.
C Fluorescently labeled F-actin (white arrow) present in TNTs between individual HPMCs. Scale bar: 20 μm.
D Scanning electron microscope image of a potential TNT precursor (black arrowhead). Insert shows a fluorescence microscopic image of filopodia-like protrusions (white arrowhead) approaching a neighboring cell. Scale bar: 2 μm.[1]
A tunneling nanotube (TNT) or membrane nanotube is a term that has been applied to cytoskeletal protrusions that extend from the plasma membrane which enable different animal cells to connect over long distances, sometimes over 100 μm between certain types of cells.[2][3][4] Tunneling nanotubes that are less than 0.7 micrometers in diameter, have an actin structure and carry portions of plasma membrane between cells in both directions. Larger TNTs (>0.7 μm) contain an actin structure with microtubules and/or intermediate filaments, and can carry components such as vesicles and organelles between cells, including whole mitochondria.[5][6][7] The diameter of TNTs ranges from 0.05 μm to 1.5 μm and they can reach lengths of several cell diameters.[7][8] There have been two types of observed TNTs: open ended and closed ended. Open ended TNTs connect the cytoplasm of two cells. Closed ended TNTs do not have continuous cytoplasm as there is a gap junction cap that only allows small molecules and ions to flow between cells.[9] These structures have shown involvement in cell-to-cell communication, transfer of nucleic acids such as mRNA and miRNA between cells in culture or in a tissue, and the spread of pathogens or toxins such as HIV and prions.[10][11][12][13][14][3] TNTs have observed lifetimes ranging from a few minutes up to several hours, and several proteins have been implicated in their formation and inhibition, including many that interact with Arp2/3.[15][16]
History
[edit]
Membrane nanotubes were first described in a 1999 Cell article examining the development of Drosophila melanogaster wing imaginal discs.[17] More recently, a Science article published in 2004 described structures that connected PC12 cells together, as well as other types of cell cultures.[7][18] This study coined the term "tunneling nanotubes" and also showed that nanotube formation between cells is correlated with both membrane and organelle transfer.[7] Since these publications, more TNT-like structures have been recorded, containing varying levels of F-actin, microtubules and other components, but remaining relatively homogenous in terms of composition.[15]
Formation
[edit]Several mechanisms may be involved in nanotube formation. These include molecular controls as well as cell-to-cell interactions.
Two primary mechanisms for TNT formation have been proposed. The first involves cytoplasmic protrusions extending from one cell to another, where they fuse with the membrane of the target cell.[7] The other mechanism occurs when two previously connected cells move away from one another, and TNTs remain as bridges between the two cells.[3][19]
Induction
[edit]Some dendritic cells and THP-1 monocytes have been shown to connect via tunneling nanotubes and display evidence of calcium flux when exposed to bacterial or mechanical stimuli. TNT-mediated signaling has shown to produce spreading in target cells, similar to the lamellipodia produced when dendritic cells are exposed to bacterial products. The TNTs demonstrated in this study propagated at initial speed of 35 micrometers/second and have shown to connect THP-1 monocytes with nanotubes up to 100 micrometers long.[20]
Phosphatidylserine exposure has demonstrated the ability to guide TNT formation from mesenchymal stem cells (MSCs) to a population of injured cells.[21] The protein S100A4 and its receptor have been shown to guide the direction of TNT growth, as p53 activates caspase 3 to cleave S100A4 in the initiating cell, thereby generating a gradient in which the target cell has higher amounts of the protein.[22] These findings suggests that chemotactic gradients may be involved in TNT induction.
One study found that cell-to-cell contact was necessary for the formation of nanotube bridges between T cells.[3] p53 activation has also been implicated as a necessary mechanism for the development of TNTs, as the downstream genes up-regulated by p53 (namely EGFR, Akt, PI3K, and mTOR) were found to be involved in nanotube formation following hydrogen peroxide treatment and serum starvation.[23] Connexin-43 has shown to promote connection between bone marrow stromal cells (BMSCs) and alveolar epithelial cells, leading to the formation of nanotubes.[24]
Cellular stress by rotenone or TNF-α was also shown to induce TNT formation between epithelial cells.[25] Inflammation by lipopolysaccharides or interferon-γ has shown to increase the expression of proteins related to TNT formation.[26]
Inhibition
[edit]While TNTs have many components, their main inhibitors work by blocking or limiting actin formation. TNT-like structures called streamers, which are extremely thin protrusions, did not form when cultured with cytochalasin D, an F-actin depolymerizing compound.[27][28] A separate study using cytochalasin B found that it impacted TNT formation without the destruction of existing TNTs.[29] Latrunculin-B, another F-actin depolymerizing compound, was found to completely block TNT formation.[7] Blocking CD38, which had been implicated in the release of mitochondria by astrocytes, also significantly decreased TNT formation.[30][31]
TNFAIP2, also called M-Sec, is known to mediate TNT formation, and knockdown of this protein by shRNA reduced TNT development in epithelial cells by about two-thirds.[26]
Inhibiting Arp2/3 directly resulted in different effects depending on cell type. In human eye cells and macrophages, blocking Arp2/3 led to a decrease in TNT formation. However, such inhibition in neuronal cells resulted in an increase in the amount of cells connected via TNTs, while lowering the total amount of TNTs connecting cells.[32]
Role in intercellular transfer
[edit]Mitochondria
[edit]Tunneling nanotubes have been implicated as one mechanism by which whole mitochondria can be transferred from cell to cell.[7] A recent study in Nature Nanotechnology has reported that cancer cells can hijack the mitochondria from immune cells via physical tunneling nanotubes.[34] Mitochondrial DNA damage appears to be the main trigger for the formation of TNTs in order to traffic entire mitochondria, though the exact threshold of damage necessary to induce TNT formation is yet unknown.[35] The maximum speed of mitochondria traveling over TNTs was found to be about 80 nm/s, lower than the measured speed of 100-1400 nm/s of axonal transport of mitochondria; this could be due to the smaller diameter of TNTs inhibiting mitochondrial migration.[36]
In one study, Ahmad et al. used four lines of mesenchymal stem cells, each expressing either a differing phenotype of the Rho-GTPase Miro1; a higher level of Miro1 was associated with more efficient mitochondrial transfer via TNTs.[25] Several studies have shown, through the selective blockage of TNT formation, that TNTs are a primary mechanism for the trafficking of whole mitochondria between heterogeneous cells.[37][38][39]
One use of this phenomenon is in the recovery from heart attacks.[40] When cardiac muscle cells are injured by oxygen deprivation, the damaged mitochondria release reactive oxygen species, which trigger nearby mesenchymal stem cells to produce and donate healthy mitochondria to the damaged muscle cells through TNTs.[40]
Action potential
[edit]Tunneling nanotubes have been shown to propagate action potentials via their extensions of endoplasmic reticulum that propagate Ca2+ influx through active diffusion.[41]
Viruses
[edit]Many viruses can transfer their proteins to TNT-connected cells. Certain types, such as influenza, have even been found to transfer their genome via TNTs.[42] Over two dozen types of viruses have been found to transfer through and/or modulate TNT.[43] A 2022 study suggests that SARS-CoV-2 builds tunneling nanotubes from nose cells to gain access to the brain.[44][45]
HIV also appears to spread through TNTs, specifically between dendritic cells.[40] Researchers have found that "Long-term nonprogressors" of HIV, who can control the virus without antiretroviral therapy, have a defect in their dendritic cells' ability to create TNTs.[40]
Prions
[edit]Prions can also spread through TNTs.[40]
Nanomedicine
[edit]Tunneling nanotubes have the potential to be involved in applications of nanomedicine, as they have shown the ability to transfer such treatments between cells. Future applications look to either inhibit TNTs to prevent nanomedicine toxicity from reaching neighboring cells, or to promote TNT formation to increase positive effects of the medicine.[46]
TNT-like structures
[edit]While TNT-like structures are all made of cytoskeletal cellular protrusions, their fundamental difference with TNTs is in the connection between two cells. TNT-like structures do not share intracellular contents such as ions or small molecules between connected cells–a feature that is present in both open ended and closed ended TNTs.[9]
A TNT-like structure called a cytoneme enables exchanges between signaling centers. The formation of cytonemes towards a FGF homolog gradient has been observed, suggesting that chemotactic controls may also induce the formation of TNT-like structures.[17] Cytonemes, however, do not always connect the membrane two cells and can act solely as environmental sensors.[28]
Plasmodesmata have been identified as functional channels interconnecting plant cells, and stromules interconnect plastids.[47][48]
Myopodia are actin-rich cytoplasmic extensions which have been observed in embryonic Drosophila. Similar structures have been observed in Xenopus and mouse models.[15] Actin-containing cellular protrusions dubbed "streamers" have been observed in cultured B cells.[28]
Vesicular transport in membrane nanotubes has been modeled utilizing a continuum approach.[49] A variety of synthetic nanotubes, based on stacking of cyclic peptides and other cyclic molecules, have been investigated.[50]
See also
[edit]References
[edit]- ^ Ranzinger J, Rustom A, Abel M, Leyh J, Kihm L, Witkowski M, et al. (2011-12-27). Bereswill S (ed.). "Nanotube action between human mesothelial cells reveals novel aspects of inflammatory responses". PLOS ONE. 6 (12): e29537. Bibcode:2011PLoSO...629537R. doi:10.1371/journal.pone.0029537. PMC 3246504. PMID 22216308.
- ^ Abounit S, Zurzolo C (March 2012). "Wiring through tunneling nanotubes--from electrical signals to organelle transfer". Journal of Cell Science. 125 (Pt 5): 1089–1098. doi:10.1242/jcs.083279. PMID 22399801. S2CID 8433589.
- ^ a b c d Sowinski S, Jolly C, Berninghausen O, Purbhoo MA, Chauveau A, Köhler K, et al. (February 2008). "Membrane nanotubes physically connect T cells over long distances presenting a novel route for HIV-1 transmission". Nature Cell Biology. 10 (2): 211–219. doi:10.1038/ncb1682. PMID 18193035. S2CID 25410308.
- ^ Davis DM, Sowinski S (June 2008). "Membrane nanotubes: dynamic long-distance connections between animal cells". Nature Reviews. Molecular Cell Biology. 9 (6): 431–436. doi:10.1038/nrm2399. PMID 18431401. S2CID 8136865.
- ^ Resnik N, Erman A, Veranič P, Kreft ME (October 2019). "Triple labelling of actin filaments, intermediate filaments and microtubules for broad application in cell biology: uncovering the cytoskeletal composition in tunneling nanotubes". Histochemistry and Cell Biology. 152 (4): 311–317. doi:10.1007/s00418-019-01806-3. PMID 31392410. S2CID 199491883.
- ^ Onfelt B, Nedvetzki S, Benninger RK, Purbhoo MA, Sowinski S, Hume AN, et al. (December 2006). "Structurally distinct membrane nanotubes between human macrophages support long-distance vesicular traffic or surfing of bacteria". Journal of Immunology. 177 (12): 8476–8483. doi:10.4049/jimmunol.177.12.8476. PMID 17142745.
- ^ a b c d e f g h Rustom A, Saffrich R, Markovic I, Walther P, Gerdes HH (February 2004). "Nanotubular highways for intercellular organelle transport". Science. 303 (5660): 1007–1010. Bibcode:2004Sci...303.1007R. doi:10.1126/science.1093133. PMID 14963329. S2CID 37863055.
- ^ Wang ZG, Liu SL, Tian ZQ, Zhang ZL, Tang HW, Pang DW (November 2012). "Myosin-driven intercellular transportation of wheat germ agglutinin mediated by membrane nanotubes between human lung cancer cells". ACS Nano. 6 (11): 10033–10041. doi:10.1021/nn303729r. PMID 23102457.
- ^ a b Zurzolo C (August 2021). "Tunneling nanotubes: Reshaping connectivity". Current Opinion in Cell Biology. Membrane Trafficking. 71: 139–147. doi:10.1016/j.ceb.2021.03.003. PMID 33866130. S2CID 233298036.
- ^ Onfelt B, Davis DM (November 2004). "Can membrane nanotubes facilitate communication between immune cells?". Biochemical Society Transactions. 32 (Pt 5): 676–678. doi:10.1042/BST0320676. PMID 15493985. S2CID 32181738.
- ^ Haimovich G, Dasgupta S, Gerst JE (February 2021). "RNA transfer through tunneling nanotubes". Biochemical Society Transactions. 49 (1): 145–160. doi:10.1042/BST20200113. PMID 33367488. S2CID 229689880.
- ^ Haimovich G, Ecker CM, Dunagin MC, Eggan E, Raj A, Gerst JE, Singer RH (November 2017). "Intercellular mRNA trafficking via membrane nanotube-like extensions in mammalian cells". Proceedings of the National Academy of Sciences of the United States of America. 114 (46): E9873–E9882. Bibcode:2017PNAS..114E9873H. doi:10.1073/pnas.1706365114. PMC 5699038. PMID 29078295.
- ^ Belting M, Wittrup A (December 2008). "Nanotubes, exosomes, and nucleic acid-binding peptides provide novel mechanisms of intercellular communication in eukaryotic cells: implications in health and disease". The Journal of Cell Biology. 183 (7): 1187–1191. doi:10.1083/jcb.200810038. PMC 2606965. PMID 19103810.
- ^ Gousset K, Schiff E, Langevin C, Marijanovic Z, Caputo A, Browman DT, et al. (March 2009). "Prions hijack tunnelling nanotubes for intercellular spread". Nature Cell Biology. 11 (3): 328–336. doi:10.1038/ncb1841. PMID 19198598. S2CID 30793469.
- ^ a b c Gurke S, Barroso JF, Gerdes HH (May 2008). "The art of cellular communication: tunneling nanotubes bridge the divide". Histochemistry and Cell Biology. 129 (5): 539–550. doi:10.1007/s00418-008-0412-0. PMC 2323029. PMID 18386044.
- ^ Hanna SJ, McCoy-Simandle K, Miskolci V, Guo P, Cammer M, Hodgson L, Cox D (August 2017). "The Role of Rho-GTPases and actin polymerization during Macrophage Tunneling Nanotube Biogenesis". Scientific Reports. 7 (1): 8547. Bibcode:2017NatSR...7.8547H. doi:10.1038/s41598-017-08950-7. PMC 5561213. PMID 28819224.
- ^ a b Ramírez-Weber FA, Kornberg TB (May 1999). "Cytonemes: cellular processes that project to the principal signaling center in Drosophila imaginal discs". Cell. 97 (5): 599–607. doi:10.1016/S0092-8674(00)80771-0. PMID 10367889. S2CID 15789546.
- ^ Onfelt B, Nedvetzki S, Yanagi K, Davis DM (August 2004). "Cutting edge: Membrane nanotubes connect immune cells". Journal of Immunology. 173 (3): 1511–1513. doi:10.4049/jimmunol.173.3.1511. PMID 15265877.
- ^ Sherer NM, Lehmann MJ, Jimenez-Soto LF, Horensavitz C, Pypaert M, Mothes W (March 2007). "Retroviruses can establish filopodial bridges for efficient cell-to-cell transmission". Nature Cell Biology. 9 (3): 310–315. doi:10.1038/ncb1544. PMC 2628976. PMID 17293854.
- ^ Watkins SC, Salter RD (September 2005). "Functional connectivity between immune cells mediated by tunneling nanotubules". Immunity. 23 (3): 309–318. doi:10.1016/j.immuni.2005.08.009. PMID 16169503.
- ^ Liu K, Ji K, Guo L, Wu W, Lu H, Shan P, Yan C (March 2014). "Mesenchymal stem cells rescue injured endothelial cells in an in vitro ischemia-reperfusion model via tunneling nanotube like structure-mediated mitochondrial transfer". Microvascular Research. 92: 10–18. doi:10.1016/j.mvr.2014.01.008. PMID 24486322.
- ^ Sun X, Wang Y, Zhang J, Tu J, Wang XJ, Su XD, et al. (December 2012). "Tunneling-nanotube direction determination in neurons and astrocytes". Cell Death & Disease. 3 (12): e438. doi:10.1038/cddis.2012.177. PMC 3542613. PMID 23222508.
- ^ Wang Y, Cui J, Sun X, Zhang Y (April 2011). "Tunneling-nanotube development in astrocytes depends on p53 activation". Cell Death and Differentiation. 18 (4): 732–742. doi:10.1038/cdd.2010.147. PMC 3131904. PMID 21113142.
- ^ Islam MN, Das SR, Emin MT, Wei M, Sun L, Westphalen K, et al. (April 2012). "Mitochondrial transfer from bone-marrow-derived stromal cells to pulmonary alveoli protects against acute lung injury". Nature Medicine. 18 (5): 759–765. doi:10.1038/nm.2736. PMC 3727429. PMID 22504485.
- ^ a b Ahmad T, Mukherjee S, Pattnaik B, Kumar M, Singh S, Kumar M, et al. (May 2014). "Miro1 regulates intercellular mitochondrial transport & enhances mesenchymal stem cell rescue efficacy". The EMBO Journal. 33 (9): 994–1010. doi:10.1002/embj.201386030. PMC 4193933. PMID 24431222.
- ^ a b Hase K, Kimura S, Takatsu H, Ohmae M, Kawano S, Kitamura H, et al. (December 2009). "M-Sec promotes membrane nanotube formation by interacting with Ral and the exocyst complex". Nature Cell Biology. 11 (12): 1427–1432. doi:10.1038/ncb1990. PMID 19935652. S2CID 1388030.
- ^ Austefjord MW, Gerdes HH, Wang X (January 2014). "Tunneling nanotubes: Diversity in morphology and structure". Communicative & Integrative Biology. 7 (1): e27934. doi:10.4161/cib.27934. PMC 3995728. PMID 24778759.
- ^ a b c Austefjord MW, Gerdes HH, Wang X (January 2014). "Tunneling nanotubes: Diversity in morphology and structure". Communicative & Integrative Biology. 7 (1): e27934. doi:10.4161/cib.27934. PMC 3995728. PMID 24778759.
- ^ Bukoreshtliev NV, Wang X, Hodneland E, Gurke S, Barroso JF, Gerdes HH (May 2009). "Selective block of tunneling nanotube (TNT) formation inhibits intercellular organelle transfer between PC12 cells". FEBS Letters. 583 (9): 1481–1488. doi:10.1016/j.febslet.2009.03.065. PMID 19345217. S2CID 13528434.
- ^ Hayakawa K, Esposito E, Wang X, Terasaki Y, Liu Y, Xing C, et al. (July 2016). "Transfer of mitochondria from astrocytes to neurons after stroke". Nature. 535 (7613): 551–555. Bibcode:2016Natur.535..551H. doi:10.1038/nature18928. PMC 4968589. PMID 27466127.
- ^ Marlein CR, Piddock RE, Mistry JJ, Zaitseva L, Hellmich C, Horton RH, et al. (May 2019). "CD38-Driven Mitochondrial Trafficking Promotes Bioenergetic Plasticity in Multiple Myeloma". Cancer Research. 79 (9): 2285–2297. doi:10.1158/0008-5472.CAN-18-0773. PMID 30622116.
- ^ Dagar S, Pathak D, Oza HV, Mylavarapu SV (November 2021). "Tunneling nanotubes and related structures: molecular mechanisms of formation and function". The Biochemical Journal. 478 (22): 3977–3998. doi:10.1042/bcj20210077. PMID 34813650. S2CID 244529025.
- ^ Ady JW, Desir S, Thayanithy V, Vogel RI, Moreira AL, Downey RJ, et al. (2014-10-31). "Intercellular communication in malignant pleural mesothelioma: properties of tunneling nanotubes". Frontiers in Physiology. 5: 400. doi:10.3389/fphys.2014.00400. PMC 4215694. PMID 25400582.
- ^ Saha T, Dash C, Jayabalan R, Khiste S, Kulkarni A, Kurmi K, et al. (January 2022). "Intercellular nanotubes mediate mitochondrial trafficking between cancer and immune cells". Nature Nanotechnology. 17 (1): 98–106. Bibcode:2022NatNa..17...98S. doi:10.1038/s41565-021-01000-4. PMC 10071558. PMID 34795441. S2CID 244349825.
- ^ Torralba D, Baixauli F, Sánchez-Madrid F (2016). "Mitochondria Know No Boundaries: Mechanisms and Functions of Intercellular Mitochondrial Transfer". Frontiers in Cell and Developmental Biology. 4: 107. doi:10.3389/fcell.2016.00107. PMC 5039171. PMID 27734015.
- ^ Wang X, Gerdes HH (July 2015). "Transfer of mitochondria via tunneling nanotubes rescues apoptotic PC12 cells". Cell Death and Differentiation. 22 (7): 1181–1191. doi:10.1038/cdd.2014.211. PMC 4572865. PMID 25571977.
- ^ Pasquier J, Guerrouahen BS, Al Thawadi H, Ghiabi P, Maleki M, Abu-Kaoud N, et al. (April 2013). "Preferential transfer of mitochondria from endothelial to cancer cells through tunneling nanotubes modulates chemoresistance". Journal of Translational Medicine. 11 (1): 94. doi:10.1186/1479-5876-11-94. PMC 3668949. PMID 23574623.
- ^ Lu J, Zheng X, Li F, Yu Y, Chen Z, Liu Z, et al. (February 2017). "Tunneling nanotubes promote intercellular mitochondria transfer followed by increased invasiveness in bladder cancer cells". Oncotarget. 8 (9): 15539–15552. doi:10.18632/oncotarget.14695. PMC 5362504. PMID 28107184.
- ^ Li X, Zhang Y, Yeung SC, Liang Y, Liang X, Ding Y, et al. (September 2014). "Mitochondrial transfer of induced pluripotent stem cell-derived mesenchymal stem cells to airway epithelial cells attenuates cigarette smoke-induced damage". American Journal of Respiratory Cell and Molecular Biology. 51 (3): 455–465. doi:10.1165/rcmb.2013-0529OC. PMID 24738760.
- ^ a b c d e Callier, Viviane (2018-04-23). "Cells Talk and Help One Another via Tiny Tube Networks". Quanta Magazine. Retrieved 2024-09-25.
- ^ Smith IF, Shuai J, Parker I (April 2011). "Active generation and propagation of Ca2+ signals within tunneling membrane nanotubes". Biophysical Journal. 100 (8): L37–L39. Bibcode:2011BpJ...100L..37S. doi:10.1016/j.bpj.2011.03.007. PMC 3077701. PMID 21504718.
- ^ Kumar A, Kim JH, Ranjan P, Metcalfe MG, Cao W, Mishina M, et al. (January 2017). "Influenza virus exploits tunneling nanotubes for cell-to-cell spread". Scientific Reports. 7 (1): 40360. Bibcode:2017NatSR...740360K. doi:10.1038/srep40360. PMC 5216422. PMID 28059146.
- ^ Jansens RJ, Tishchenko A, Favoreel HW (March 2020). Glaunsinger BA (ed.). "Bridging the Gap: Virus Long-Distance Spread via Tunneling Nanotubes". Journal of Virology. 94 (8): e02120–19. doi:10.1128/JVI.02120-19. PMC 7108841. PMID 32024778.
- ^ "Coronavirus may enter the brain by building tiny tunnels from the nose". New Scientist. Retrieved 23 August 2022.
- ^ Pepe A, Pietropaoli S, Vos M, Barba-Spaeth G, Zurzolo C (July 2022). "Tunneling nanotubes provide a route for SARS-CoV-2 spreading". Science Advances. 8 (29): eabo0171. Bibcode:2022SciA....8O.171P. doi:10.1126/sciadv.abo0171. PMC 9299553. PMID 35857849.
- ^ Ottonelli I, Caraffi R, Tosi G, Vandelli MA, Duskey JT, Ruozi B (February 2022). "Tunneling Nanotubes: A New Target for Nanomedicine?". International Journal of Molecular Sciences. 23 (4): 2237. doi:10.3390/ijms23042237. PMC 8878036. PMID 35216348.
- ^ Gallagher KL, Benfey PN (January 2005). "Not just another hole in the wall: understanding intercellular protein trafficking". Genes & Development. 19 (2): 189–195. doi:10.1101/gad.1271005. PMID 15655108.
- ^ Köhler RH, Cao J, Zipfel WR, Webb WW, Hanson MR (June 1997). "Exchange of protein molecules through connections between higher plant plastids". Science. 276 (5321): 2039–2042. doi:10.1126/science.276.5321.2039. PMID 9197266.
- ^ Kuznetsov AV (August 2011). "Modeling bidirectional transport of quantum dot nanoparticles in membrane nanotubes". Mathematical Biosciences. 232 (2): 101–109. doi:10.1016/j.mbs.2011.04.008. PMID 21609723.
- ^ Rodríguez-Vázquez N, Fuertes A, Amorín M, Granja JR (2016). "Bioinspired Artificial Sodium and Potassium Ion Channels". In Sigel A, Sigel H, Sigel RK (eds.). The Alkali Metal Ions: Their Role for Life. Metal Ions in Life Sciences. Vol. 16. pp. 485–556. doi:10.1007/978-3-319-21756-7_14. ISBN 978-3-319-21755-0. PMID 26860310.
Further reading
[edit]- Gurke S, Barroso JF, Gerdes HH (May 2008). "The art of cellular communication: tunneling nanotubes bridge the divide". Histochemistry and Cell Biology. 129 (5): 539–550. doi:10.1007/s00418-008-0412-0. PMC 2323029. PMID 18386044.
- "Tunnelling nanotubes: Life's secret network". New Scientist. November 2008.
External links
[edit]- Hans-Hermann Gerdes Research Group - The laboratory that first observed membrane nanotubes


 French
French Deutsch
Deutsch