Nebivolol
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Nebilet, Bystolic, others |
| Other names | Narbivolol, Nebivolol, Nebivololum[1] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a608029 |
| License data | |
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Protein binding | 98% |
| Metabolism | Liver (CYP2D6-mediated) |
| Elimination half-life | 12-19 hours[2][3][4] |
| Excretion | Kidney and fecal |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| Chemical and physical data | |
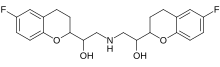
| Formula | C22H25F2NO4 |
| Molar mass | 405.442 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |

Nebivolol is a beta blocker used to treat high blood pressure and heart failure.[5] As with other β-blockers, it is generally a less preferred treatment for high blood pressure.[6] It may be used by itself or with other blood pressure medication.[6] It is taken by mouth.[6]
Common side effects include dizziness, feeling tired, nausea, and headaches.[6] Serious side effects may include heart failure and bronchospasm.[6] Its use in pregnancy and breastfeeding is not recommended.[5][7] It works by blocking β1-adrenergic receptors in the heart and dilating blood vessels.[6][8]
Nebivolol was patented in 1983 and came into medical use in 1997.[9] It is available as a generic medication in the United Kingdom.[5] In 2022, it was the 173rd most commonly prescribed medication in the United States, with more than 3 million prescriptions.[10][11]
Medical uses
[edit]It is used to treat high blood pressure and heart failure.[5] Nebivolol is used in the treatment of angina, to decrease the heart rate and contractile force. This is relevant in patients who need to decrease the oxygen demand of the heart so that the blood supplied from stenosed or constricted arteries is adequate.
ACE inhibitors, angiotensin II receptor antagonists, calcium-channel blockers, and thiazide diuretics are generally preferred over beta blockers for the treatment of primary hypertension in the absence of co-morbidities.[12][13][14][15]
Pharmacology and biochemistry
[edit]β1-selectivity
[edit]Beta blockers help patients with cardiovascular disease by blocking β1 receptors, while many of the side-effects of these medications are caused by their blockade of β2 receptors.[16] For this reason, beta blockers that selectively block β1 adrenergic receptors (termed cardioselective or β1-selective beta blockers) produce fewer adverse effects (for instance, bronchoconstriction) than those drugs that non-selectively block both β1 and β2 receptors.
In a laboratory experiment conducted on biopsied heart tissue, nebivolol proved to be the most β1-selective of the β-blockers tested, being approximately 3.5 times more β1-selective than bisoprolol.[17] However, the drug's receptor selectivity in humans is more complex and depends on the drug dose and the genetic profile of the patient taking the medication.[18] The drug is highly cardioselective at 5 mg.[19] In addition, at doses above 10 mg, nebivolol loses its cardioselectivity and blocks both β1 and β2 receptors,[18] while the recommended starting dose of nebivolol is 5 mg, sufficient control of blood pressure may require doses up to 40 mg.[18] Furthermore, nebivolol is also not cardioselective when taken by patients with a genetic makeup that makes them "poor metabolizers" of nebivolol (and other drugs) or with CYP2D6 inhibitors.[18] As many as 1 in 10 Caucasian people and even more black people are poor CYP2D6 metabolizers and therefore might benefit less from nebivolol's cardioselectivity although currently there are no directly comparable studies.[citation needed]
Nebivolol[20] while selectively blocking beta(1) receptor acts as a beta(3)-agonist. β3 receptors are found in the gallbladder, urinary bladder, and in brown adipose tissue. Their role in gallbladder physiology is unknown, but they are thought to play a role in lipolysis and thermogenesis in brown fat. In the urinary bladder it is thought to cause relaxation of the bladder and prevention of urination.[21][22][23]
Due to enzymatic inhibition, fluvoxamine increases the exposure to nebivolol and its active hydroxylated metabolite (4-OH-nebivolol) in healthy volunteers.[24]
Vasodilator action
[edit]Nebivolol is unique as a beta-blocker.[25] Unlike carvedilol, it has a nitric oxide (NO)-potentiating, vasodilatory effect via stimulation of β3 receptors.[26][27][28]
Nebivolol induces vasodilation by stimulating the production of nitric oxide, a natural blood vessel relaxant. This effect is achieved by activating the endothelial isoform of NO synthase (eNOS) in the cells lining the blood vessels. Unlike traditional β-blockers, nebivolol's unique mechanism of action improves arterial flexibility and reduces peripheral resistance, making it beneficial for hypertensive patients with endothelial dysfunction. The drug's ability to increase NO production persists even after metabolism, offering long-lasting benefits. Nebivolol's distinct approach to promoting NO release has shown promising results in improving endothelial function and managing hypertension in clinical trials.[29]
Along with labetalol, celiprolol and carvedilol, it is one of four beta blockers to cause dilation of blood vessels in addition to effects on the heart.[28]
Antihypertensive effect
[edit]Nebivolol lowers blood pressure (BP) by reducing peripheral vascular resistance, and significantly increases stroke volume with preservation of cardiac output.[30] The net hemodynamic effect of nebivolol is the result of a balance between the depressant effects of beta-blockade and an action that maintains cardiac output.[31] Antihypertensive responses were significantly higher with nebivolol than with placebo in trials enrolling patient groups considered representative of the U.S. hypertensive population, in black people, and in those receiving concurrent treatment with other antihypertensive drugs.[32]
Pharmacokinetics
[edit]Nebivolol plasma protein binding is approximately 98%, mostly to albumin and its half-life of low doses is 12 hours in extensive CYP2D6 metabolizers and 19 hours in poor metabolizers.[33]
Contraindications
[edit]- Severe bradycardia
- Heart block greater than first degree
- Patients with cardiogenic shock
- Decompensated cardiac failure
- Sick sinus syndrome (unless a permanent pacemaker is in place)
- Patients with severe hepatic impairment (Child-Pugh class B)
- Patients who are hypersensitive to any component of this product.
Side effects
[edit]Side effects might include headache, tiredness, dizziness, lightheadedness, reduced blood flow to extremities, bradycardia.[34]
Controversies
[edit]Pharmacology of side-effects
[edit]Several studies have suggested that nebivolol has reduced typical beta-blocker-related side effects, such as fatigue, clinical depression, bradycardia, or impotence.[35][36][37] However, according to the FDA[38]
Bystolic is associated with a number of serious risks. Bystolic is contraindicated in patients with severe bradycardia, heart block greater than first degree, cardiogenic shock, decompensated cardiac failure, sick sinus syndrome (unless a permanent pacemaker is in place), severe hepatic impairment (Child-Pugh > B) and in patients who are hypersensitive to any component of the product. Bystolic therapy is also associated with warnings regarding abrupt cessation of therapy, cardiac failure, angina and acute myocardial infarction, bronchospastic diseases, anesthesia and major surgery, diabetes and hypoglycemia, thyrotoxicosis, peripheral vascular disease, non-dihydropyridine calcium channel blockers use, as well as precautions regarding use with CYP2D6 inhibitors, impaired renal and hepatic function, and anaphylactic reactions. Finally, Bystolic is associated with other risks as described in the Adverse Reactions section of its PI. For example, a number of treatment-emergent adverse events with an incidence greater than or equal to 1 percent in Bystolic-treated patients and at a higher frequency than placebo-treated patients were identified in clinical studies, including headache, fatigue, and dizziness.
FDA warning letter about advertising claims
[edit]In August 2008, the FDA issued a Warning Letter to Forest Laboratories citing exaggerated and misleading claims in their launch journal ad, in particular over claims of superiority and novelty of action.[38]
History
[edit]Mylan Laboratories licensed the US and Canadian rights to nebivolol from Janssen Pharmaceutica N.V. in 2001. Nebivolol is already registered and successfully marketed in more than 50 countries, including the United States where it is marketed under the brand name Bystolic from Mylan Laboratories and Forest Laboratories. Nebivolol is manufactured by Forest Laboratories.
In India, nebivolol is available as Nebula (Zydus Healthcare Ltd), Nebizok (Eris life-sciences), Nebicip (Cipla ltd), Nebilong (Micro Labs), Nebistar (Lupin ltd), Nebicard (Torrent), Nubeta (Abbott Healthcare Pvt Ltd – India), and Nodon (Cadila Pharmaceuticals).
In Greece and Italy, nebivolol is marketed by Menarini as Lobivon.
In Germany it is marketed as Nebilet by Berlin Chemie.
In the Middle East, Russia and Australia, it is marketed under the name Nebilet and in Pakistan it is marketed by The Searle Company Limited as Byscard.
References
[edit]- ^ "Nebivolol". go.drugbank.com. Retrieved 17 August 2022.
- ^ "Drugs@FDA: FDA-Approved Drugs Nebivolol - ALLERGAN" (PDF). accessdata.fda.gov. Retrieved 17 August 2022.
- ^ Giles TD, Cockcroft JR, Pitt B, Jakate A, Wright HM (September 2017). "Rationale for nebivolol/valsartan combination for hypertension: review of preclinical and clinical data". Journal of Hypertension. 35 (9): 1758–1767. doi:10.1097/HJH.0000000000001412. PMC 5548499. PMID 28509722.
- ^ "DrugBank Nebivolol". go.drugbank.com. Retrieved 17 August 2022.
- ^ a b c d British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. p. 154. ISBN 9780857113382.
- ^ a b c d e f "Nebivolol Hydrochloride Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Retrieved 3 March 2019.
- ^ "Nebivolol Pregnancy and Breastfeeding Warnings". Drugs.com. Retrieved 3 March 2019.
- ^ de Boer RA, Voors AA, van Veldhuisen DJ (July 2007). "Nebivolol: third-generation beta-blockade". Expert Opinion on Pharmacotherapy. 8 (10): 1539–1550. doi:10.1517/14656566.8.10.1539. PMID 17661735. S2CID 24186687.
- ^ Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 462. ISBN 9783527607495.
- ^ "The Top 300 of 2022". ClinCalc. Archived from the original on 30 August 2024. Retrieved 30 August 2024.
- ^ "Nebivolol Drug Usage Statistics, United States, 2013 - 2022". ClinCalc. Retrieved 30 August 2024.
- ^ Reboussin DM, Allen NB, Griswold ME, Guallar E, Hong Y, Lackland DT, et al. (June 2018). "Systematic Review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". Hypertension. 71 (6): e116–e135. doi:10.1161/HYP.0000000000000067. PMID 29133355. S2CID 34462045.
- ^ Fretheim A, Odgaard-Jensen J, Brørs O, Madsen S, Njølstad I, Norheim OF, et al. (April 2012). "Comparative effectiveness of antihypertensive medication for primary prevention of cardiovascular disease: systematic review and multiple treatments meta-analysis". BMC Medicine. 10 (1): 33. doi:10.1186/1741-7015-10-33. PMC 3354999. PMID 22480336.
- ^ Seleme VB, Marques GL, Mendes AE, Rotta I, Pereira M, Júnior EL, da Cunha CL (March 2021). "Nebivolol for the Treatment of Essential Systemic Arterial Hypertension: A Systematic Review and Meta-Analysis". American Journal of Cardiovascular Drugs. 21 (2): 165–180. doi:10.1007/s40256-020-00422-0. PMID 32710438. S2CID 220732879.
- ^ National Heart Foundation of Australia. National Blood Pressure and Vascular DiseaseAdvisory Committee (2016). Guideline for the diagnosis and management of hypertension in adults. Melbourne, Vic. ISBN 978-1-74345-110-6. OCLC 970693159.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Tafreshi MJ, Weinacker AB (August 1999). "Beta-adrenergic-blocking agents in bronchospastic diseases: a therapeutic dilemma". Pharmacotherapy. 19 (8): 974–978. doi:10.1592/phco.19.11.974.31575. PMID 10453968. S2CID 32202416.
- ^ Bundkirchen A, Brixius K, Bölck B, Nguyen Q, Schwinger RH (January 2003). "Beta 1-adrenoceptor selectivity of nebivolol and bisoprolol. A comparison of [3H]CGP 12.177 and [125I]iodocyanopindolol binding studies". European Journal of Pharmacology. 460 (1): 19–26. doi:10.1016/S0014-2999(02)02875-3. PMID 12535855.
- ^ a b c d "Prescribing information for Bystolic". Forest Laboratories, Inc. Archived from the original (PDF) on 25 March 2016. Retrieved 11 June 2009.
- ^ Nuttall SL, Routledge HC, Kendall MJ (June 2003). "A comparison of the beta1-selectivity of three beta1-selective beta-blockers". Journal of Clinical Pharmacy and Therapeutics. 28 (3): 179–186. doi:10.1046/j.1365-2710.2003.00477.x. PMID 12795776. S2CID 58760796.
- ^ Rozec B, Erfanian M, Laurent K, Trochu JN, Gauthier C (April 2009). "Nebivolol, a vasodilating selective beta(1)-blocker, is a beta(3)-adrenoceptor agonist in the nonfailing transplanted human heart". Journal of the American College of Cardiology. 53 (17): 1532–1538. doi:10.1016/j.jacc.2008.11.057. PMID 19389564.
- ^ Sawa M, Harada H (2006). "Recent developments in the design of orally bioavailable beta3-adrenergic receptor agonists". Current Medicinal Chemistry. 13 (1): 25–37. doi:10.2174/092986706775198006. PMID 16457637.
- ^ Ferrer-Lorente R, Cabot C, Fernández-López JA, Alemany M (September 2005). "Combined effects of oleoyl-estrone and a beta3-adrenergic agonist (CL316,243) on lipid stores of diet-induced overweight male Wistar rats". Life Sciences. 77 (16): 2051–2058. doi:10.1016/j.lfs.2005.04.008. PMID 15935402.
- ^ Rang HP, Dale MM, Ritter JM, Moore PK (2003). Pharmacology (5th ed.). Edinburgh: Churchill Livingstone. p. 163. ISBN 0-443-07145-4.
- ^ Gheldiu AM, Vlase L, Popa A, Briciu C, Muntean D, Bocsan C, et al. (2017). "Investigation of a Potential Pharmacokinetic Interaction Between Nebivolol and Fluvoxamine in Healthy Volunteers". Journal of Pharmacy & Pharmaceutical Sciences. 20: 68–80. doi:10.18433/J3B61H. PMID 28459657.
- ^ Agabiti Rosei E, Rizzoni D (2007). "Metabolic profile of nebivolol, a beta-adrenoceptor antagonist with unique characteristics". Drugs. 67 (8): 1097–1107. doi:10.2165/00003495-200767080-00001. PMID 17521213. S2CID 25807936.
- ^ Karimi Galougahi K, Liu CC, Garcia A, Gentile C, Fry NA, Hamilton EJ, et al. (February 2016). "β3 Adrenergic Stimulation Restores Nitric Oxide/Redox Balance and Enhances Endothelial Function in Hyperglycemia". Journal of the American Heart Association. 5 (2): e002824. doi:10.1161/JAHA.115.002824. PMC 4802476. PMID 26896479.
- ^ Weiss R (2006). "Nebivolol: a novel beta-blocker with nitric oxide-induced vasodilatation". Vascular Health and Risk Management. 2 (3): 303–308. doi:10.2147/vhrm.2006.2.3.303. PMC 1993984. PMID 17326335.
- ^ a b Bakris G (May 2009). "An in-depth analysis of vasodilation in the management of hypertension: focus on adrenergic blockade". Journal of Cardiovascular Pharmacology. 53 (5): 379–387. doi:10.1097/FJC.0b013e31819fd501. PMID 19454898. S2CID 205598744.
- ^ Maffei A, Lembo G (August 2009). "Nitric oxide mechanisms of nebivolol". Therapeutic Advances in Cardiovascular Disease. 3 (4): 317–327. doi:10.1177/1753944709104496. PMID 19443516.
- ^ Kamp O, Sieswerda GT, Visser CA (August 2003). "Comparison of effects on systolic and diastolic left ventricular function of nebivolol versus atenolol in patients with uncomplicated essential hypertension". The American Journal of Cardiology. 92 (3): 344–348. doi:10.1016/S0002-9149(03)00645-3. PMID 12888152.
- ^ Gielen W, Cleophas TJ, Agrawal R (August 2006). "Nebivolol: a review of its clinical and pharmacological characteristics". International Journal of Clinical Pharmacology and Therapeutics. 44 (8): 344–357. doi:10.5414/cpp44344. PMID 16961165.
- ^ Baldwin CM, Keam SJ (2009). "Nebivolol: in the treatment of hypertension in the US". American Journal of Cardiovascular Drugs. 9 (4): 253–260. doi:10.2165/1120274-000000000-00000. PMID 19655820. S2CID 12785427.
- ^ "RxAbbVie - BYSTOLIC® (nebivolol) tablets, for oral use Full Prescribing Information" (PDF). www.rxabbvie.com. January 2019. Retrieved 17 August 2022.
- ^ "Nebivolol Oral: Uses, Side Effects, Interactions, Pictures, Warnings & Dosing - WebMD". www.webmd.com. Retrieved 17 August 2022.
- ^ Pessina AC (December 2001). "Metabolic effects and safety profile of nebivolol". Journal of Cardiovascular Pharmacology. 38. 38 (Suppl 3): S33–S35. doi:10.1097/00005344-200112003-00006. PMID 11811391. S2CID 20786564.
- ^ Weber MA (December 2005). "The role of the new beta-blockers in treating cardiovascular disease". American Journal of Hypertension. 18 (12 Pt 2): 169S–176S. doi:10.1016/j.amjhyper.2005.09.009. PMID 16373195.
- ^ Poirier L, Cléroux J, Nadeau A, Lacourcière Y (August 2001). "Effects of nebivolol and atenolol on insulin sensitivity and haemodynamics in hypertensive patients". Journal of Hypertension. 19 (8): 1429–1435. doi:10.1097/00004872-200108000-00011. PMID 11518851. S2CID 35105142.
- ^ a b Thomas Abrams (28 August 2008). "Warning Letter" (PDF). Food and Drug Administration. Archived from the original (PDF) on 28 April 2017. Retrieved 16 December 2019.
FDA is not aware of any substantial evidence or substantial clinical experience that demonstrates that Bystolic represents a 'novel' or 'next generation' beta blocker for the treatment of hypertension. Indeed, we are not aware of any well-designed trials comparing Bystolic to other β-blockers. Furthermore, FDA is not aware of any data that would render Bystolic's mechanism of action 'unique.'


 French
French Deutsch
Deutsch