Mastitis
| Mastitis | |
|---|---|
| Other names | mammitis; garget |
 | |
| Colorized photo illustrating mastitis, 1908 | |
| Pronunciation | |
| Specialty | Gynecology |
| Symptoms | Localized breast pain and redness, fever[1] |
| Complications | Abscess[2] |
| Usual onset | Rapid[1] |
| Diagnostic method | Based on symptoms[2] |
| Differential diagnosis | Plugged milk duct,[3] breast engorgement,[4] breast cancer (rare)[1] |
| Prevention | Frequent breastfeeding with good technique[2] |
| Treatment | Antibiotics (cephalexin), ibuprofen[2][1] |
| Frequency | 10% of breastfeeding women[2] |
Mastitis is inflammation of the breast or udder, usually associated with breastfeeding.[1][5][6] Symptoms typically include local pain and redness.[1] There is often an associated fever and general soreness.[1] Onset is typically fairly rapid and usually occurs within the first few months of delivery.[1] Complications can include abscess formation.[2]
Risk factors include poor latch, cracked nipples, use of a breast pump, and weaning.[1] The bacteria most commonly involved are Staphylococcus and Streptococci.[1] Diagnosis is typically based on symptoms.[2] Ultrasound may be useful for detecting a potential abscess.[1]
Prevention of this breastfeeding difficulty is by proper breastfeeding techniques.[2] When infection is present, antibiotics such as cephalexin may be recommended.[2] Breastfeeding should typically be continued, as emptying the breast is important for healing.[2][1] Tentative evidence supports benefits from probiotics.[1] About 10% of breastfeeding women are affected.[2]
Types
[edit]When it occurs in breastfeeding mothers, it is known as puerperal mastitis, lactation mastitis, or lactational mastitis. When it occurs in non breastfeeding women it is known as non-puerperal or non-lactational mastitis. Mastitis can, in rare cases, occur in men. Inflammatory breast cancer has symptoms very similar to mastitis and must be ruled out.
The symptoms are similar for puerperal and nonpuerperal mastitis but predisposing factors and treatment can be very different.
Pregnancy related
[edit]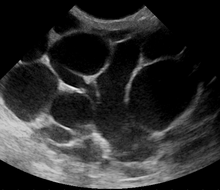
Puerperal mastitis is the inflammation of the breast in connection with pregnancy, breastfeeding or weaning. Since one of the most prominent symptoms is tension and engorgement of the breast, it is thought to be caused by blocked milk ducts or milk excess. It is relatively common; estimates range depending on methodology between 5–33%. However, only about 0.4–0.5% of breastfeeding mothers develop an abscess.[7]
Some predisposing factors are known but their predictive value is minimal. It appears that proper breastfeeding technique, frequent breastfeeding and avoidance of stress are the most important factors that can be influenced.
Light cases of mastitis are often called breast engorgement; the distinction is overlapping and possibly arbitrary or subject to regional variations.
Non-pregnancy related
[edit]The term nonpuerperal mastitis describes inflammatory lesions of the breast occurring unrelated to pregnancy and breastfeeding. This article includes description of mastitis as well as various kinds of mammary abscesses. Skin related conditions like dermatitis and foliculitis are a separate entity.
Names for non-puerperal mastitis are not used very consistently and include mastitis, subareolar abscess, duct ectasia, periductal inflammation, Zuska's disease and others.
Periductal mastitis is a form of nonlactational mastitis, and is characterized by inflammation of the subareolar ducts. Although the cause of periductal mastitis is currently unknown, it is predicted that smoking may be related. This condition is mainly seen in young women but can also be seen in men.[8]
Signs and symptoms
[edit]
Lactation mastitis usually affects only one breast and the symptoms can develop quickly.[9] It develops into three stages, from the initial stage, the pus formation stage, to the restoration stage.[10] The signs and symptoms usually appear suddenly and they include:
- Breast tenderness or warmth to the touch
- General malaise or feeling ill
- Swelling of the breast
- Pain or a burning sensation continuously or while breast-feeding
- Skin redness, often in a wedge-shaped pattern
- Fever of 101 F (38.3 C) or greater[11]
- The affected breast can then start to appear lumpy and red.
Some women may also experience flu-like symptoms such as:
Contact should be made with a health care provider with special breastfeeding competence as soon as the patient recognizes the combination of signs and symptoms. Most of the women first experience the flu-like symptoms and just after they may notice a sore red area on the breast. Also, women should seek medical care if they notice any abnormal discharge from the nipples, if breast pain is making it difficult to function each day, or they have prolonged, unexplained breast pain.[citation needed]
Breast abscess
[edit]

A breast abscess is a collection of pus that develops in the breast with various causes.[13] During lactation, breast abscess develops only rarely, most sources cite about 0.4–0.5% of breastfeeding women.[7] Known risk factors are age over 30, primiparous (first birth) and late delivery. No correlation was found with smoking status; however, this may be in part because far fewer smoking women choose to breastfeed.[14] Antibiotics were not shown effective in prevention of lactation abscess but are useful to treat a secondary infection (see the section on the treatment of breast abscess in this article).
Keratinizing squamous metaplasia of lactiferous ducts may play a similar[clarification needed] role in the pathogenesis of nonpuerperal subareolar abscess.
Causes
[edit]Since the 1980s mastitis has often been divided into non-infectious and infectious sub-groups. However, recent research [15] suggests that it may not be feasible to make divisions in this way. It has been shown that types and amounts of potentially pathogenic bacteria in breast milk are not correlated to the severity of symptoms. Moreover, although only 15% of women with mastitis in Kvist et al.'s study were given antibiotics, all recovered and few had recurring symptoms. Many healthy breastfeeding women wishing to donate breast milk have potentially pathogenic bacteria in their milk but have no symptoms of mastitis.[citation needed]
Risk factors
[edit]Mastitis typically develops when the milk is not properly removed from the breast. Milk stasis can lead to the milk ducts in the breasts becoming blocked, as the breast milk is not being properly and regularly expressed.[16] It has also been suggested that blocked milk ducts can occur as a result of pressure on the breast, such as tight-fitting clothing or an over-restrictive bra, although there is sparse evidence for this supposition. Mastitis may occur when the baby is not appropriately attached to the breast while feeding, when the baby has infrequent feeds or has problems suckling the milk out of the breast.
The presence of cracks or sores on the nipples increases the likelihood of infection. There is a possibility that infants carrying infectious pathogens in their noses can infect their mothers;[17] the clinical significance of this finding is still unknown.
Mastitis can also develop due to contamination of a breast implant or any other foreign body, for example after nipple piercing. In such cases, the removal of the foreign body is indicated.[18]
Women who are breastfeeding are at risk for developing mastitis especially if they have sore or cracked nipples or have had mastitis before while breastfeeding another baby. Also, the chances of getting mastitis increases if women use only one position to breastfeed or wear a tight-fitting bra, which may restrict milk flow [19] Difficulties in getting a nursing infant to latch on to the breast can also increase the risk for mastitis.[20]
Women with diabetes, chronic illness, AIDS, or an impaired immune system may be more susceptible to the development of mastitis.[21]
Infection
[edit]Some women (approximately 15%)[15] will require antibiotic treatment for infection which is usually caused by bacteria from the skin or the baby's mouth entering the milk ducts through skin lesions of the nipple or through the opening of the nipple.[22] Infection is usually caused by Staphylococcus aureus.[23] Infectious pathogens commonly associated with mastitis are Staphylococcus aureus, Streptococcus spp. and Gram-negative bacilli such as Escherichia coli. Salmonella spp., mycobacteria, and fungi such as Candida and Cryptococcus have been identified in rare instances.[7]
Recent research suggests that infectious pathogens play a much smaller role in the pathogenesis than was commonly assumed only a few years ago. Most detected pathogens are very common species that are natural part of the breast fauna and simple detection of their presence is not sufficient to prove a causative role. Furthermore, there are indications that treatment with antibiotics may have minimal impact,[24][25] and over-all there is insufficient evidence to confirm or refute the effectiveness of antibiotic therapy for treating lactational mastitis.[26]
Diagnosis
[edit]The diagnosis of mastitis and breast abscess can usually be made based on a physical examination.[23] The doctor will also take into account the signs and symptoms of the condition.
However, if the doctor is not sure whether the mass is an abscess or a tumor, a breast ultrasound may be performed. The ultrasound provides a clear image of the breast tissue and may be helpful in distinguishing between simple mastitis and abscess or in diagnosing an abscess deep in the breast. The test consists of placing an ultrasound probe over the breast.
In cases of infectious mastitis, cultures may be needed in order to determine what type of organism is causing the infection. Cultures are helpful in deciding the specific type of antibiotics that will be used in curing the disease. These cultures may be taken either from the breast milk or of the material aspirated from an abscess.
Mammograms or breast biopsies are normally performed on women who do not respond to treatment or on non-breastfeeding women. This type of tests is sometimes ordered to exclude the possibility of a rare type of breast cancer which causes symptoms similar to those of mastitis.
Differential diagnosis
[edit]Perinatal mood and anxiety disorders
[edit]Some women who experience pain or other symptoms when breastfeeding, but who have no detectable signs of mastitis, may have a sensory processing disorder, postpartum depression, perinatal anxiety, dysphoric milk ejection reflex, an involuntary aversion to breastfeeding, or other mental health problems.[27]
Breast cancer
[edit]Breast cancer may coincide with or mimic symptoms of mastitis. Only full resolution of symptoms and careful examination are sufficient to exclude the diagnosis of breast cancer.
The lifetime risk for breast cancer is significantly reduced for women who were pregnant and breastfeeding. Mastitis episodes do not appear to influence lifetime risk of breast cancer.[citation needed]
Mastitis does however cause great difficulties in diagnosis of breast cancer. Breast cancer may coincide with mastitis or develop shortly afterwards. All suspicious symptoms that do not completely disappear within 5 weeks must be investigated.[citation needed]
Breast cancer incidence during pregnancy and lactation is assumed to be the same as in controls. Course and prognosis are also very similar to age matched controls.[28][29] However diagnosis during lactation is particularly problematic, often leading to delayed diagnosis and treatment.
Some data suggest that noninflammatory breast cancer incidence is increased within a year following episodes of nonpuerperal mastitis and special care is required for follow-up cancer prevention screening.[30] So far only data from short term observation is available and total risk increase can not be judged. Because of the very short time between presentation of mastitis and breast cancer in this study it is considered very unlikely that the inflammation had any substantial role in carcinogenesis, rather it would appear that some precancerous lesions may increase the risk of inflammation (hyperplasia causing duct obstruction, hypersensitivity to cytokines or hormones) or the lesions may have common predisposing factors.
A very serious type of breast cancer called inflammatory breast cancer presents with similar symptoms as mastitis (both puerperal and nonpuerperal). It is the most aggressive type of breast cancer with the highest mortality rate. The inflammatory phenotype of IBC is thought to be mostly caused by invasion and blocking of dermal lymphatics, however it was recently shown that NF-κB target genes activation may significantly contribute to the inflammatory phenotype. Case reports show that inflammatory breast cancer symptoms can flare up following injury or inflammation making it even more likely to be mistaken for mastitis. Symptoms are also known to partially respond to progesterone and antibiotics, reaction to other common medications can not be ruled out at this point.[31][32][33][34][35]
Treatment
[edit]Lactational mastitis
[edit]When mastitis is associated with breastfeeding, the treatment has to balance short-term reduction of symptoms with solving the underlying problems that caused mastitis. For example, the Academy of Breastfeeding Medicine recommends against trying to "empty" the breasts, whether through pushing the baby to feed more or through using a breast pump.[27] It may reduce the feeling of being full or swollen in the short term, at the cost of triggering milk oversupply, which can cause a mastitis recurrence in the coming days and weeks.[27]
Self-care
[edit]For breastfeeding women with breast engorgement or light mastitis, using a warm compress may be comfortable.[27] However, by increasing blood flow to the area, warm compresses make the symptoms worse for other women.[27] A cool compresses can reduce edema (swelling) and pain.[27] In traditional folk medicine, the breast was sometimes cooled by placing a cabbage leaf on the breast, but this is now more commonly done with an ice pack or a wet washcloth.[27]
Gentle massage ("like petting a cat"[27]) may be comfortable and may reduce swelling.[27] However, more aggressive rubbing can easily damage breast tissues that are already strained by mastitis, and that damage can increase swelling and pain.[27] Excessive massage, like excessive use of a breast pump, may be a risk factor for recurrent mastitis.[27]
Probiotics may or may not help, but they are believed not to be harmful.[27] Over-the-counter nonsteroidal anti-inflammatory drugs, such as ibuprofen and paracetamol, may reduce inflammation.[27]
Medical treatments
[edit]Antibiotics are appropriate only for bacterial mastitis, which may develop if non-infective mastitis does not improve.[27] Antifungals are similarly only useful when a fungal infection, such as thrush, is present.[27] Severe infections may require ordinary medical supportive care, such as intravenous fluids if the mother is unable to drink enough water or other fluids.[27]
Therapeutic ultrasound may reduce swelling.[27]
Ineffective and harmful treatments
[edit]The shape of swelling in a specific spot may make people suppose that the breasts contain simple tubes, and that one has become plugged. However, milk ducts are not simple tubes, and their interconnected anatomy makes it impossible for them to actually become plugged.[27] Consequently, treatment does not include cutting, popping, or squeezing any so-called "plugged" ducts.[27] There is no "plug" (e.g., of dried-out milk) to be removed.[27] These localized swellings are usually caused by lymphatic congestion (non-milk body fluid accumulating in the breasts), alveolar edema (swelling in the part of the breast that produces milk), or mammary dysbiosis (changes to the breast's microbiome), which can cause some narrowing, but not plugging, at the microscopic level.[27] Breastfeeding at a normal level may provide temporary relief from the swelling without triggering milk oversupply.[27] It is safer to treat nipple blebs (very small, usually pale colored, bumps of tissue on the end of the nipple) with topical steroids than by cutting the skin.[27]
Any action that breaks the skin can cause an infection, which increases inflammation and may become serious.[27]
Antibiotics do not prevent mastitis from recurring.[27][36]
Nonpuerperal mastitis
[edit]Nonpuerperal mastitis is treated by medication and possibly aspiration or drainage (see in particular treatment of subareolar abscess and treatment of granulomatous mastitis). According to a BMJ best practice report, antibiotics are generally to be used in all mastitis cases unrelated to breastfeeding, with replacement of the antibiotics by an antifungal agent such as fluconazole in cases of deep fungal infections, and corticosteroids are to be used in case of granulomatous mastitis (with differential diagnosis to tuberculosis infection of the breast).[18]
In idiopathic granulomatous mastitis, successful treatment includes invasive surgical procedures or less invasive treatment with steroid medications.[37]
Antibiotics for bacterial mastitis
[edit]In lactational mastitis, antibiotics are not needed in the overwhelming majority of cases and should be used only for bacterial infections.[24] For people with non-severe infections, dicloxacillin or cephalexin are recommended.[38] For people with severe infections, vancomycin is recommended.[39] The length of antibiotic treatment ranges anywhere from 5–14 days.[40] The effects of antibiotics has not been well studied as of 2013.[41]
A lactational phlegmon (area of inflammation) should be monitored for possible development into an abscess (walled-off area filled with pus from an infection).[27]
Breast abscess
[edit]An abscess (or suspected abscess) in the breast may be treated by ultrasound-guided fine-needle aspiration (percutaneous aspiration) or by surgical incision and drainage; each of these approaches is performed under antibiotic coverage. In case of puerperal breast abscess, breastfeeding from the affected breast should be continued where possible.[24][42]
For small breast abscesses, ultrasound-guided fine needle aspiration such as to completely drain the abscess is widely recognized as a preferred initial management.[43]
One recommended treatment includes antibiotics, ultrasound evaluation and, if fluid is present, ultrasound-guided fine needle aspiration of the abscess with an 18 gauge needle, under saline lavage until clear.[44] The exudate is then sent for microbiological analysis for identification of the pathogen and determination of its antibiotic sensitivity profile,[45] which may in turn give an indication for changing the antibiotics. At follow-up, a mammography is performed if the condition has resolved; otherwise the ultrasound-guided fine-needle aspiration with lavage and microbiological analysis is repeated.[46] If three to five aspirations still do not resolve the condition, percutaneous drainage in combination with placement of an indwelling catheter is indicated, and only if several attempts at ultrasound-guided drainage fail, surgical resection of the inflamed lactiferous ducts (preferably performed after the acute episode is over).[47] It is noted, however, that even the excision of the affected ducts does not necessarily prevent recurrence.[47]
Nonpuerperal breast abscesses have a higher rate of recurrence compared to puerperal breast abscesses.[48] There is a high statistical correlation of nonpuerperal breast abscess with diabetes mellitus (DM). On this basis, it has recently been suggested that diabetes screening should be performed on patients with such abscess.[49][50]
Although there are a number of recommendations regarding the treatment of breast abscesses, a 2015 review found insufficient evidence of whether needle aspiration is comparable to incision and drainage, or whether antibiotics should generally be given to women undergoing incision and drainage.[51]
Prevention
[edit]Most efforts to prevent mastitis in breastfeeding women are believed to be ineffective or have a relatively small effect.[36] Acupoint massage probably reduces the risk somewhat.[36] Possibly effective prevention measures include taking probiotics, breast massage, and low-frequency pulse treatment.[36] Ineffective methods included prophylactic antibiotics, topical treatments (mastitis is inflammation deep in the breast, so treating the skin is irrelevant[27]), specialist breastfeeding education, and anti‐secretory factor‐inducing cereal.[36]
Prognosis
[edit]Neither the presence of a fever nor the severity of symptoms at presentation do not predict outcome; women with sore or damaged nipples may need special attention.[52][53]
Epidemiology
[edit]Mastitis is quite common among breastfeeding women. The WHO estimates that although incidences vary between 2.6% and 33%, the prevalence globally is approximately 10% of breastfeeding women. Most mothers who develop mastitis usually do so within the first few weeks after delivery. Most breast infections occur within the first or second month after delivery or at the time of weaning.[21] However, in rare cases it affects women who are not breastfeeding.[54]
Terminology
[edit]Popular usage of the term mastitis varies by geographic region. Outside the US, it is commonly used for both puerperal (that is, occurring to breastfeeding mothers) and nonpuerperal (unrelated to breastfeeding) cases. In the US, mastitis usually refers to puerperal mastitis with fever or other symptoms of systemic infection (these symptoms are not necessarily caused by an actual infection[27]). Lighter cases of puerperal mastitis, appearing a few days after birth, are often called breast engorgement.[27] In the US, the term nonpuerperal mastitis is rarely used, and alternative names such as duct ectasia, subareolar abscess and plasma cell mastitis are more frequently used.
In this article, mastitis is used in the original sense of the definition as inflammation of the breast, with additional qualifiers where appropriate.
Chronic cystic mastitis is an older name for fibrocystic breast changes.
Etymology and pronunciation
[edit]The word mastitis (/mæstˈaɪtɪs/) uses combining forms of mast- + -itis. The word mammitis (/mæmˈaɪtɪs/) uses combining forms of mamm- + -itis. They are synonymous in modern usage, and mastitis is the more commonly used synonym.
Other animals
[edit]Mastitis occurs in other animals as in humans, and is especially a concern in livestock, since milk from the affected udders of livestock may enter the food supply and pose a health risk.
It is a major condition in some species, like dairy cows. It is the cause of much unwanted suffering for the dairy cows. It is of tremendous economic importance for the dairy industry, and it is also of concern for public health. The same considerations apply to mastitis in sheep and goats and other milk-producing females. It is also of economic importance in the sow, but, in this species, it is not related to public health. In other domestic females (queen, mare, etc.), it is more an individual illness dealt with by veterinary practitioners.
- Udder of a Roux du Valais sheep after a healed mastitis; one teat was lost due to the disease.
- Serous exudate from bovine udder in E. coli mastitis[55] at left. Normal milk at right.
- Gangrenous mastitis in a dairy cow.
- Cat with mastitis
See also
[edit]- Galactocele, a milk-filled cyst
References
[edit]- ^ a b c d e f g h i j k l m Berens PD (December 2015). "Breast Pain: Engorgement, Nipple Pain, and Mastitis". Clinical Obstetrics and Gynecology. 58 (4): 902–14. doi:10.1097/GRF.0000000000000153. PMID 26512442. S2CID 13006527.
- ^ a b c d e f g h i j k Spencer JP (September 2008). "Management of mastitis in breastfeeding women". American Family Physician. 78 (6): 727–31. PMID 18819238.
- ^ Ferri FF (2009). Ferri's Clinical Advisor 2010 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 593. ISBN 978-0-323-07685-2.
- ^ Buttaro TM, Trybulski J, Bailey PP, Sandberg-Cook J (2007). Primary Care: A Collaborative Practice. Elsevier Health Sciences. p. PT1608. ISBN 978-0-323-07841-2.
- ^ The Worldwatch Institute (2015). State of the World 2006: Special Focus: China and India. Island Press. p. 36. ISBN 978-1-61091-633-2.
- ^ Ratcliffe SD (2008). Family Medicine Obstetrics. Elsevier Health Sciences. p. 634. ISBN 978-0-323-04306-9.
- ^ a b c Michie C, Lockie F, Lynn W (September 2003). "The challenge of mastitis". Archives of Disease in Childhood. 88 (9): 818–21. doi:10.1136/adc.88.9.818. PMC 1719627. PMID 12937109.
- ^ Dixon JM, Pariser KM. "Nonlactational mastitis in adults". UpToDate. Retrieved 2019-08-02.
- ^ "Symptoms of mastitis". Retrieved 2010-04-20.
- ^ Zhang Y, Sun X, Li K, Wang X, Cai L, Li X, Zhou M (2018-05-02). ""The Therapy of Elimination First" for Early Acute Mastitis: A Systematic Review and Meta-Analysis". Evidence-Based Complementary and Alternative Medicine. 2018: 8059256. doi:10.1155/2018/8059256. PMC 5954910. PMID 29853971.
- ^ "Symptoms". Retrieved 2010-04-20.
- ^ "Breast Infection Symptoms". Retrieved 2010-04-20.
- ^ Segura-Sampedro JJ, Jiménez-Rodríguez R, Camacho-Marente V, Pareja-Ciuró F, Padillo-Ruiz J (May 2016). "Breast abscess and sepsis arising from oral infection". Cirugia Espanola. 94 (5): 308–9. doi:10.1016/j.ciresp.2015.05.007. PMID 26148851.
- ^ Cusack L, Brennan M (December 2011). "Lactational mastitis and breast abscess - diagnosis and management in general practice". Australian Family Physician. 40 (12): 976–9. PMID 22146325.
- ^ a b Kvist LJ, Larsson BW, Hall-Lord ML, Steen A, Schalén C (April 2008). "The role of bacteria in lactational mastitis and some considerations of the use of antibiotic treatment". International Breastfeeding Journal. 3 (1): 6. doi:10.1186/1746-4358-3-6. PMC 2322959. PMID 18394188.
- ^ "Non-infectious mastitis and milk stasis". Archived from the original on 2010-04-28. Retrieved 2010-04-20.
- ^ Amir LH, Garland SM, Lumley J (October 2006). "A case-control study of mastitis: nasal carriage of Staphylococcus aureus". BMC Family Practice. 7: 57. doi:10.1186/1471-2296-7-57. PMC 1630426. PMID 17032458.
- ^ a b Mastitis and breast abscess Archived 2009-06-12 at the Wayback Machine, BMJ Best Practice (last updated 5 September 2014) (subscription-limited access)
- ^ "Risk factors". Retrieved 2010-04-20.
- ^ "Common questions about breastfeeding and pain". womenshealth.gov. Archived from the original on 4 August 2017. Retrieved 4 August 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ a b "Breast Infection Causes". Retrieved 2010-04-20.
- ^ "Breastfeeding Mastitis Causes and Symptoms". Archived from the original on 2019-07-19. Retrieved 2010-04-20.
- ^ a b "Exams and Tests". Retrieved 2010-04-20.
- ^ a b c Peters J (April 2004). "[Mastitis puerperalis - causes and therapy]". Zentralblatt für Gynäkologie (in German). 126 (2): 73–6. doi:10.1055/s-2004-44880. PMID 15112132. S2CID 7649157.
- ^ Barbosa-Cesnik C, Schwartz K, Foxman B (April 2003). "Lactation mastitis". JAMA. 289 (13): 1609–12. doi:10.1001/jama.289.13.1609. PMID 12672715.
- ^ Antibiotics for mastitis in breastfeeding women. Cochrane Database of Systematic Reviews, PubMed Health. Review published 2013; Review content assessed as up-to-date: November 23, 2012.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac Mitchell KB, Johnson HM, Rodríguez JM, Eglash A, Scherzinger C, Zakarija-Grkovic I, et al. (May 2022). "Academy of Breastfeeding Medicine Clinical Protocol #36: The Mastitis Spectrum, Revised 2022". Breastfeeding Medicine. 17 (5): 360–376. doi:10.1089/bfm.2022.29207.kbm. PMID 35576513. S2CID 248832395.
- ^ Middleton LP, Amin M, Gwyn K, Theriault R, Sahin A (September 2003). "Breast carcinoma in pregnant women: assessment of clinicopathologic and immunohistochemical features". Cancer. 98 (5): 1055–60. doi:10.1002/cncr.11614. PMID 12942575. S2CID 21424443.
- ^ Shousha S (July 2000). "Breast carcinoma presenting during or shortly after pregnancy and lactation". Archives of Pathology & Laboratory Medicine. 124 (7): 1053–60. doi:10.5858/2000-124-1053-BCPDOS. PMID 10888783.
- ^ Peters F, Kiesslich A, Pahnke V (October 2002). "Coincidence of nonpuerperal mastitis and noninflammatory breast cancer". European Journal of Obstetrics, Gynecology, and Reproductive Biology. 105 (1): 59–63. doi:10.1016/S0301-2115(02)00109-4. PMID 12270566.
- ^ Kusama M, Koyanagi Y, Sekine M, Serizawa H, Ebihara Y, Hirota T, Nakamura Y, Matsunaga T (September 1994). "[A case of inflammatory breast cancer successfully treated with 5'-DFUR and MPA]". Gan to Kagaku Ryoho. Cancer & Chemotherapy (in Japanese). 21 (12): 2049–52. PMID 8085857.
- ^ Yamada T, Okazaki M, Okazaki A, Sato H, Watanabe Y, Toda K, Okazaki Y, Asaishi K, Hirata K, Narimatsu E (September 1992). "[A case of inflammatory breast cancer treated with medroxyprogesterone acetate (MPA) in combination with intra-arterial infusion chemotherapy]". Gan to Kagaku Ryoho. Cancer & Chemotherapy (in Japanese). 19 (11): 1923–5. PMID 1387777.
- ^ Van Laere SJ, Van der Auwera I, Van den Eynden GG, Elst HJ, Weyler J, Harris AL, van Dam P, Van Marck EA, Vermeulen PB, Dirix LY (June 2006). "Nuclear factor-kappaB signature of inflammatory breast cancer by cDNA microarray validated by quantitative real-time reverse transcription-PCR, immunohistochemistry, and nuclear factor-kappaB DNA-binding". Clinical Cancer Research. 12 (11 Pt 1): 3249–56. doi:10.1158/1078-0432.CCR-05-2800. PMID 16740744. S2CID 86034806.
- ^ Van Laere SJ, Van der Auwera I, Van den Eynden GG, van Dam P, Van Marck EA, Vermeulen PB, Dirix LY (September 2007). "NF-kappaB activation in inflammatory breast cancer is associated with oestrogen receptor downregulation, secondary to EGFR and/or ErbB2 overexpression and MAPK hyperactivation". British Journal of Cancer. 97 (5): 659–69. doi:10.1038/sj.bjc.6603906. PMC 2360371. PMID 17700572.
- ^ van der Burg B, van der Saag PT (June 1996). "Nuclear factor-kappa-B/steroid hormone receptor interactions as a functional basis of anti-inflammatory action of steroids in reproductive organs". Molecular Human Reproduction. 2 (6): 433–8. doi:10.1093/molehr/2.6.433. PMID 9238713.
- ^ a b c d e Crepinsek MA, Taylor EA, Michener K, Stewart F, et al. (Cochrane Pregnancy and Childbirth Group) (September 2020). "Interventions for preventing mastitis after childbirth". The Cochrane Database of Systematic Reviews. 2020 (9): CD007239. doi:10.1002/14651858.CD007239.pub4. PMC 8094918. PMID 32987448.
- ^ Lei X, Chen K, Zhu L, Song E, Su F, Li S (September 2017). "Treatments for Idiopathic Granulomatous Mastitis: Systematic Review and Meta-Analysis". Breastfeeding Medicine. 12 (7): 415–421. doi:10.1089/bfm.2017.0030. PMID 28731822.
- ^ Spencer JP (September 2008). "Management of mastitis in breastfeeding women". American Family Physician (review). 78 (6): 727–731. PMID 18819238.
- ^ David MZ, Daum RS (2017). "Treatment of Staphylococcus aureus Infections". Staphylococcus aureus. Current Topics in Microbiology and Immunology. Vol. 409. pp. 325–383. doi:10.1007/82_2017_42. ISBN 978-3-319-72061-6. PMID 28900682.
- ^ Jahanfar S, Ng CJ, Teng CL (2016). "Antibiotics for mastitis in breastfeeding women". Sao Paulo Medical Journal = Revista Paulista de Medicina. 134 (3): 273. doi:10.1590/1516-3180.20161343T1. PMC 10496608. PMID 27355802.
- ^ Jahanfar S, Ng CJ, Teng CL (February 2013). "Antibiotics for mastitis in breastfeeding women". The Cochrane Database of Systematic Reviews (2): CD005458. doi:10.1002/14651858.CD005458.pub3. PMC 11297410. PMID 23450563.
- ^ Trop I, Dugas A, David J, El Khoury M, Boileau JF, Larouche N, Lalonde L (October 2011). "Breast abscesses: evidence-based algorithms for diagnosis, management, and follow-up". Radiographics (review). 31 (6): 1683–99. doi:10.1148/rg.316115521. PMID 21997989., p. 1684
- ^ Silberman AW, Silberman AW (28 March 2012). Principles and Practice of Surgical Oncology: A Multidisciplinary Approach to Difficult Problems. Lippincott Williams & Wilkins. p. 301. ISBN 978-1-4511-5323-1.
- ^ Trop I, Dugas A, David J, El Khoury M, Boileau JF, Larouche N, Lalonde L (October 2011). "Breast abscesses: evidence-based algorithms for diagnosis, management, and follow-up". Radiographics (review). 31 (6): 1683–99. doi:10.1148/rg.316115521. PMID 21997989., Fig. 9 on p. 1696
- ^ Trop I, Dugas A, David J, El Khoury M, Boileau JF, Larouche N, Lalonde L (October 2011). "Breast abscesses: evidence-based algorithms for diagnosis, management, and follow-up". Radiographics (review). 31 (6): 1683–99. doi:10.1148/rg.316115521. PMID 21997989., p. 1691
- ^ Trop I, Dugas A, David J, El Khoury M, Boileau JF, Larouche N, Lalonde L (October 2011). "Breast abscesses: evidence-based algorithms for diagnosis, management, and follow-up". Radiographics (review). 31 (6): 1683–99. doi:10.1148/rg.316115521. PMID 21997989., p. 1692–1693
- ^ a b Trop I, Dugas A, David J, El Khoury M, Boileau JF, Larouche N, Lalonde L (October 2011). "Breast abscesses: evidence-based algorithms for diagnosis, management, and follow-up". Radiographics (review). 31 (6): 1683–99. doi:10.1148/rg.316115521. PMID 21997989., p. 1694
- ^ Trop I, Dugas A, David J, El Khoury M, Boileau JF, Larouche N, Lalonde L (October 2011). "Breast abscesses: evidence-based algorithms for diagnosis, management, and follow-up". Radiographics (review). 31 (6): 1683–99. doi:10.1148/rg.316115521. PMID 21997989., abstract
- ^ Rizzo M, Gabram S, Staley C, Peng L, Frisch A, Jurado M, Umpierrez G (March 2010). "Management of breast abscesses in nonlactating women". The American Surgeon. 76 (3): 292–5. doi:10.1177/000313481007600310. PMID 20349659. S2CID 25120670.
- ^ Verghese BG, Ravikanth R (May 2012). "Breast abscess, an early indicator for diabetes mellitus in non-lactating women: a retrospective study from rural India". World Journal of Surgery. 36 (5): 1195–8. doi:10.1007/s00268-012-1502-7. PMID 22395343. S2CID 23073438.
- ^ Irusen H, Rohwer AC, Steyn DW, Young T (August 2015). "Treatments for breast abscesses in breastfeeding women". The Cochrane Database of Systematic Reviews. 2015 (8): CD010490. doi:10.1002/14651858.CD010490.pub2. hdl:10019.1/104306. PMC 9226721. PMID 26279276.
- ^ Kvist LJ, Hall-Lord ML, Larsson BW (January 2007). "A descriptive study of Swedish women with symptoms of breast inflammation during lactation and their perceptions of the quality of care given at a breastfeeding clinic". International Breastfeeding Journal. 2: 2. doi:10.1186/1746-4358-2-2. PMC 1784075. PMID 17244353.
- ^ Kvist LJ, Hall-Lord ML, Rydhstroem H, Larsson BW (June 2007). "A randomised-controlled trial in Sweden of acupuncture and care interventions for the relief of inflammatory symptoms of the breast during lactation". Midwifery. 23 (2): 184–95. doi:10.1016/j.midw.2006.02.003. PMID 17052823.
- ^ "Causes of mastitis". NHS. Archived from the original on 2010-04-28. Retrieved 2010-04-20.
- ^ Kandasamy S, Green BB, Benjamin AL, Kerr DE (Dec 2011). "Between-cow variation in dermal fibroblast response to lipopolysaccharide reflected in resolution of inflammation during Escherichia coli mastitis". J. Dairy Sci. 94 (12): 5963–75. doi:10.3168/jds.2011-4288. PMID 22118085.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
External links
[edit]- Mastitis on mayoclinic.com
- Australian Breastfeeding Association


 French
French Deutsch
Deutsch
![Serous exudate from bovine udder in E. coli mastitis[55] at left. Normal milk at right.](http://upload.wikimedia.org/wikipedia/commons/thumb/b/b2/Mamite_%C3%A5_colibacile_laecea.jpg/200px-Mamite_%C3%A5_colibacile_laecea.jpg)

