Mycobacteroides abscessus
| Mycobacteroides abscessus | |
|---|---|
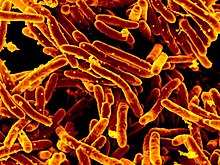 | |
| GD01 strain of Mycobacteroides abscessus isolated from patient | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Actinomycetota |
| Class: | Actinomycetia |
| Order: | Mycobacteriales |
| Family: | Mycobacteriaceae |
| Genus: | Mycobacteroides |
| Species: | M. abscessus |
| Binomial name | |
| Mycobacteroides abscessus (Moore and Frerichs 1953) Gupta et al. 2018[1] | |
| Type strain[2] | |
| ATCC 19977 CCUG 20993 CIP 104536 DSM 43491 DSM 44196 Hauduroy L948 JCM 13569 L948 NCTC 13031 TMC 1543 | |
| Subspecies | |
| |
| Synonyms[1] | |
| |
Mycobacteroides abscessus (formerly Mycobacterium abscessus[1]) is a species of rapidly growing, multidrug-resistant, nontuberculous mycobacteria (NTM) that is a common soil and water contaminant. Although M. abscessus most commonly causes chronic lung infection and skin and soft tissue infection (SSTI), it can also cause infection in almost all human organs, mostly in patients with suppressed immune systems.[3] Amongst NTM species responsible for disease, infection caused by M. abscessus complex are more difficult to treat due to antimicrobial drug resistance.[4]

Description
[edit]Mycobacteroides abscessus cells are Gram-positive, nonmotile, acid-fast rods about 1.0–2.5 μm long by 0.5 μm wide. They may form colonies on Löwenstein–Jensen medium that appear smooth or rough, white or greyish, and nonphotochromogenic.[citation needed]
Etymology
[edit]Abscessus is named for abscesses. It is a Latin word derived from ab- ("away") + cedere ("to go") because it was the ancient medical notion that a manifestation of the four humors was for pus to leave the body. M. abscessus was first isolated from gluteal abscesses in a 62-year-old patient who had injured her knee as a child and had a disseminated infection 48 years later. The species M. bolletii, which was first described in 2006, is named after the late eminent French microbiologist and taxonomist Claude Bollet.[citation needed]
Physiology
[edit]M. abscessus shows growth at 28 °C and 37 °C after 7 days, but not at 43 °C. It may grow on MacConkey agar at 28 °C and even 37 °C. It shows tolerance to saline media (5% NaCl) and 500 mg/L hydroxylamine (Ogawa egg medium) and 0.2% picrate (Sauton agar medium). Strains of the species have been shown to degrade the antibiotic p-aminosalicylate. M. abscessus has also been shown to produce arylsulfatase, but not of nitrate reductase and Tween 80 hydrolase. It shows a negative result for the iron uptake test and no use of fructose, glucose, oxalate, or citrate as sole carbon sources.[citation needed]
Differential characteristics
[edit]M. abscessus and M. chelonae can be distinguished from M. fortuitum or M. peregrinum by their failure to reduce nitrate and to take up iron. Tolerance to 5% NaCl in Löwenstein-Jensen medium, tolerance to 0.2% picrate in Sauton agar, and non-use of citrate as a sole carbon source are characteristics that distinguish M. abscessus from M. chelonae. M. abscessus and M. chelonae sequevar I share an identical sequence in the 54-510 region of 16S rRNA, though both species can be differentiated by their hsp65, ITS or rpoB gene sequences.[citation needed]
Genetics
[edit]A draft genome sequence of M. abscessus subsp. bolletii BDT was completed in 2012.[5] Since then, a large number of strains from this subspecies have had their genomes sequenced, leading to a clarification of subspecies boundaries. In 1992, M. abscessus was first recognised as a distinct species. In 2006, this group was separated into three subspecies: M. a. abscessus, M. a. bolletii, and M. a. massiliense. In 2011, the latter two were briefly merged into a single subspecies,[6] but were subsequently separated again following greater availability of genome sequence data, which showed the three subspecies formed genetically distinct groups.[7][8] It has been proposed that M. bolletii and M. massiliense be reinstated as unique species.[9]
These distinct groups also correspond to important biological differences. Clinically important differences include differing susceptibilities to antibiotics. M. a. abscessus and M. a. bolletii carry a common antibiotic resistance gene, which confers resistance to macrolide antibiotics, while M. a. massiliense is thought to carry a nonfunctional copy, so is more susceptible to antibiotics and more easily treated.[7]
Pathogenesis
[edit]M. abscessus can cause lung disease, skin infections, central nervous system infections, bacteremia, eye infections, and other, less common diseases.[7]
Chronic lung disease occurs most commonly in vulnerable hosts with underlying lung disease such as cystic fibrosis, bronchiectasis, and prior tuberculosis. Clinical symptoms of lung infection vary in scope and intensity, but commonly include chronic cough, often with purulent sputum. Haemoptysis may also be present. Systemic symptoms include malaise, fatigue, and weight loss in advanced disease.[10] The diagnosis of M. abscessus pulmonary infection requires the presence of symptoms, radiologic abnormalities, and microbiologic cultures.[citation needed]
M. abscessus can cause skin infections in immunodeficient patients, patients who have recently undergone surgery, tattooing, or acupuncture, or after exposure to hot springs or spas.[7] It can be associated with middle-ear infections (otitis media).[11]
The incidence of M. abscessus infections appears to be increasing over time.[7][12] Outbreaks of M. abscessus have been reported in hospitals and clinical settings worldwide.[13] While outbreaks of major clinical concern involve transmission (most likely indirect transmission) between vulnerable patients such as those receiving lung transplants or being treated for cystic fibrosis, outbreaks have also been reported at clinics providing cosmetic surgery, liposuction, mesotherapy and IV infusion of cell therapy, although these are more attributable to contaminated disinfectants, saline and instruments than contact between patients.[7]
Management
[edit]Bacteriophage therapy
[edit]A study from 2019 supported the capability of phages in killing resistant bacteria unable to be treated with antibiotics.[14] Research laboratories came together to find these phages by collecting, isolating, and exposing them to resistant M. abscessus that had been isolated from a patient in London.[14]
In vitro
[edit]A bacteriophage known as Muddy had proved effective at killing the patient’s distinct M. abscessus strain (GD01), while phages like ZoeJ and BPs had reduced capabilities at infecting GD01.[14] A mixture of phages, Muddy and engineered versions of ZoeJ and BPs, though, completely infected and killed GD01.[14]
In vivo
[edit]A cocktail of bacteriophages, Muddy, ZoeJ, and BPs, effectively killed a strain of M. abscessus in vitro.[14] The potential this showed encouraged the commencement of patient treatments towards the GD01 infection.[14] Every 12 hours, the patient received a treatment of the bacteriophage cocktail.[14]
One day of treatment showed high bacteriophage levels in the bloodstream.[14] This suggested that they were being released into the bloodstream and replicating to infect bacteria.[14] No significant side effects were reported.[14] The right phages were found for this patient, but a different strain may be sensitive to different phages.[14]
Type strain
[edit]The type strain of M. abscessus, most commonly referred to as ATCC 19977, was isolated in 1953 from a human knee infection presenting with abscess-like lesions, leading to the strain being named "abscessus".[15] The strain wasn't recognised as a distinct species until 1992, however, when DNA hybridisation work identified it as genetically distinct from its relative, M. chelonae.[16] The genome of the type train was published in 2009.[17]
References
[edit]This article incorporates public domain text from the CDC as cited
- ^ a b c Gupta, Radhey S.; Lo, Brian; Son, Jeen (2018-02-13). "Phylogenomics and Comparative Genomic Studies Robustly Support Division of the Genus Mycobacterium into an Emended Genus Mycobacterium and Four Novel Genera". Frontiers in Microbiology. 9: 67. doi:10.3389/fmicb.2018.00067. ISSN 1664-302X. PMC 5819568. PMID 29497402.
- ^ Euzéby JP, Parte AC. "Mycobacteroides abscessus". List of Prokaryotic names with Standing in Nomenclature (LPSN). Retrieved June 24, 2022.
- ^ Song, Joon Young; Sohn, Jang Wook; Jeong, Hye Won; Cheong, Hee Jin; Kim, Woo Joo; Kim, Min Ja (2006-01-13). "An outbreak of post-acupuncture cutaneous infection due to Mycobacterium abscessus". BMC Infectious Diseases. 6: 6. doi:10.1186/1471-2334-6-6. ISSN 1471-2334. PMC 1361796. PMID 16412228.
- ^ Lee; et al. (2015). "Mycobacterium abscesses complex infections in humans". Emerg Infect Dis. 21 (9): 1638–1646. doi:10.3201/2109.141634. PMC 4550155. PMID 26295364.
- ^ Choi, G.-E.; Cho, Y.-J.; Koh, W.-J.; Chun, J.; Cho, S.-N.; Shin, S. J. (24 April 2012). "Draft Genome Sequence of Mycobacterium abscessus subsp. bolletii BDT". Journal of Bacteriology. 194 (10): 2756–2757. doi:10.1128/JB.00354-12. PMC 3347169. PMID 22535937.
- ^ Leao, SC; Tortoli, E; Euzéby, JP; Garcia, MJ (September 2011). "Proposal that Mycobacterium massiliense and Mycobacterium bolletii be united and reclassified as Mycobacterium abscessus subsp. bolletii comb. nov., designation of Mycobacterium abscessus subsp. abscessus subsp. nov. and emended description of Mycobacterium abscessus". International Journal of Systematic and Evolutionary Microbiology. 61 (Pt 9): 2311–3. doi:10.1099/ijs.0.023770-0. PMID 21037035.
- ^ a b c d e f Lee, Meng-Rui; Sheng, Wang-Huei; Hung, Chien-Ching; Yu, Chong-Jen; Lee, Li-Na; Hsueh, Po-Ren (September 2015). "Mycobacterium abscessus Complex Infections in Humans". Emerging Infectious Diseases. 21 (9): 1638–46. doi:10.3201/2109.141634. PMC 4550155. PMID 26295364.
- ^ Tortoli E, Kohl TA, Brown-Elliott BA, Trovato A, Leao SC, Garcia MJ, Vasireddy S, Turenne CY, Griffith DE, Philley JV, Baldan R, Campana S, Cariani L, Colombo C, Taccetti G, Teri A, Niemann S, Wallace Jr RJ, Cirillo DM. (2016). "Emended description of Mycobacterium abscessus, Mycobacterium abscessus subsp. abscessus and Mycobacterium abscessus subsp. bolletiiand designation of Mycobacterium abscessus subsp. massiliense comb. nov". Int J Syst Evol Microbiol. 66 (11): 4471–4479. doi:10.1099/ijsem.0.001376. PMID 27499141.
- ^ Sassi M, Drancourt M. (2014). "Genome analysis reveals three genomospecies in Mycobacterium abscessus". BMC Genomics. 15 (1): 359. doi:10.1186/1471-2164-15-359. PMC 4035080. PMID 24886480.
- ^ Johnson; Odell (2014). "Nontuberculous mycobacterial pulmonary infections". J Thorac Dis. 6 (3): 210–220. doi:10.3978/j.issn.2072-1439.2013.12.24. PMC 3949190. PMID 24624285.
- ^ Linmans JJ, Stokroos RJ, Linssen CF (September 2008). "Mycobacterium abscessus, an uncommon cause of chronic otitis media: A case report and literature review". Arch. Otolaryngol. Head Neck Surg. 134 (9): 1004–6. doi:10.1001/archotol.134.9.1004. PMID 18794448.[permanent dead link]
- ^ Marras, Theodore K.; Mendelson, David; Marchand-Austin, Alex; May, Kevin; Jamieson, Frances B. (November 2013). "Pulmonary Nontuberculous Mycobacterial Disease, Ontario, Canada, 1998–2010". Emerging Infectious Diseases. 19 (11): 1889–1891. doi:10.3201/eid1911.130737. PMC 3837646. PMID 24210012.
- ^ Bryant, Josephine M.; Grogono, Dorothy M.; Rodriguez-Rincon, Daniela; Everall, Isobel; Brown, Karen P.; Moreno, Pablo; Verma, Deepshikha; Hill, Emily; Drijkoningen, Judith; Gilligan, Peter; Esther, Charles R.; Noone, Peadar G.; Giddings, Olivia; Bell, Scott C.; Thomson, Rachel; Wainwright, Claire E.; Coulter, Chris; Pandey, Sushil; Wood, Michelle E.; Stockwell, Rebecca E.; Ramsay, Kay A.; Sherrard, Laura J.; Kidd, Timothy J.; Jabbour, Nassib; Johnson, Graham R.; Knibbs, Luke D.; Morawska, Lidia; Sly, Peter D.; Jones, Andrew; Bilton, Diana; Laurenson, Ian; Ruddy, Michael; Bourke, Stephen; Bowler, Ian C. J. W.; Chapman, Stephen J.; Clayton, Andrew; Cullen, Mairi; Dempsey, Owen; Denton, Miles; Desai, Maya; Drew, Richard J.; Edenborough, Frank; Evans, Jason; Folb, Jonathan; Daniels, Thomas; Humphrey, Helen; Isalska, Barbara; Jensen-Fangel, Søren; Jönsson, Bodil; Jones, Andrew M.; Katzenstein, Terese L.; Lillebaek, Troels; MacGregor, Gordon; Mayell, Sarah; Millar, Michael; Modha, Deborah; Nash, Edward F.; O’Brien, Christopher; O’Brien, Deirdre; Ohri, Chandra; Pao, Caroline S.; Peckham, Daniel; Perrin, Felicity; Perry, Audrey; Pressler, Tania; Prtak, Laura; Qvist, Tavs; Robb, Ali; Rodgers, Helen; Schaffer, Kirsten; Shafi, Nadia; van Ingen, Jakko; Walshaw, Martin; Watson, Danie; West, Noreen; Whitehouse, Joanna; Haworth, Charles S.; Harris, Simon R.; Ordway, Diane; Parkhill, Julian; Floto, R. Andres (10 November 2016). "Emergence and spread of a human-transmissible multidrug-resistant nontuberculous mycobacterium". Science. 354 (6313): 751–757. Bibcode:2016Sci...354..751B. doi:10.1126/science.aaf8156. PMC 5142603. PMID 27846606.
- ^ a b c d e f g h i j k "Engineered phages treat drug-resistant infection". National Institutes of Health (NIH). 2019-05-20. Retrieved 2019-11-06.
- ^ Moore, Morris; Frerichs, John B. (February 1953). "An Unusual Acid-Fast Infection of the Knee with Subcutaneous, Abscess-Like Lesions of the Gluteal Region". Journal of Investigative Dermatology. 20 (2): 133–169. doi:10.1038/jid.1953.18. PMID 13035193.
- ^ Kusunoki, S.; Ezaki, T.; et al. (1992). "Proposal of Mycobacterium peregrinum sp. nov., nom. rev., and elevation of Mycobacterium chelonae subsp. abscessus (Kubica et al.) to species status: Mycobacterium abscessus comb. nov". Int. J. Syst. Bacteriol. 42 (2): 240–245. doi:10.1099/00207713-42-2-240. PMID 1581184.
- ^ Ripoll, Fabienne; Pasek, Sophie; Schenowitz, Chantal; Dossat, Carole; Barbe, Valérie; Rottman, Martin; Macheras, Edouard; Heym, Beate; Herrmann, Jean-Louis; Daffé, Mamadou; Brosch, Roland; Risler, Jean-Loup; Gaillard, Jean-Louis; Ahmed, Niyaz (19 June 2009). "Non Mycobacterial Virulence Genes in the Genome of the Emerging Pathogen Mycobacterium abscessus". PLOS ONE. 4 (6): e5660. Bibcode:2009PLoSO...4.5660R. doi:10.1371/journal.pone.0005660. PMC 2694998. PMID 19543527.


 French
French Deutsch
Deutsch